How can drug dosage adjustments be optimized to accommodate individual patient profiles in the context of combination therapy?
Drug dosage can significantly impact the efficacy of drug combinations. The appropriate dosage is crucial for achieving the desired therapeutic effect while minimizing side effects and reducing the risk of drug resistance. Drug dosage adjustments are essential when prescribing combination therapies, especially for patients with varying physiological conditions or comorbidities.
To optimize drug dosage adjustments for individual patient profiles in the context of combination therapy, several factors should be considered:
1.Pharmacokinetics (PK) and pharmacodynamics (PD): Understanding how a drug interacts with other drugs at the molecular level can help determine the optimal dosage for each agent. This includes factors such as absorption, distribution, metabolism, excretion, and target engagement.
2.Disease state: Different diseases have unique pathophysiology, which may require different drug combinations and dosages. For example, some conditions may benefit from high-dose therapy, while others may respond better to low-dose combinations.
3.Genetic factors: Genetic variations among individuals can influence drug response, leading to differences in efficacy and safety profiles. Tailoring drug dosages based on genetic information can improve treatment outcomes and reduce adverse events.
4.Age and gender: Age and gender can also affect drug responses, requiring specific dosage adjustments. For instance, elderly patients may need lower doses due to reduced organ function, while women may require higher doses during pregnancy or menstruation.
5.Organ impairment: Impaired liver or kidney function can alter drug clearance, necessitating dose adjustments to maintain effective concentrations.
6.Drug interactions: Knowing potential drug interactions, including synergistic, antagonistic, or additive effects, can help guide dosage adjustments.
7.Patient compliance: Ensuring that patients adhere to their medication regimen is crucial for successful combination therapy. Non-adherence can lead to suboptimal drug exposure, reduced efficacy, and increased risk of adverse events.
8.Therapeutic drug monitoring (TDM): TDM involves measuring drug levels in the bloodstream to determine if the prescribed dosage is sufficient to achieve the desired therapeutic effect. This information can then be used to adjust dosages accordingly, ensuring that patients receive the right amount of each drug in the combination.
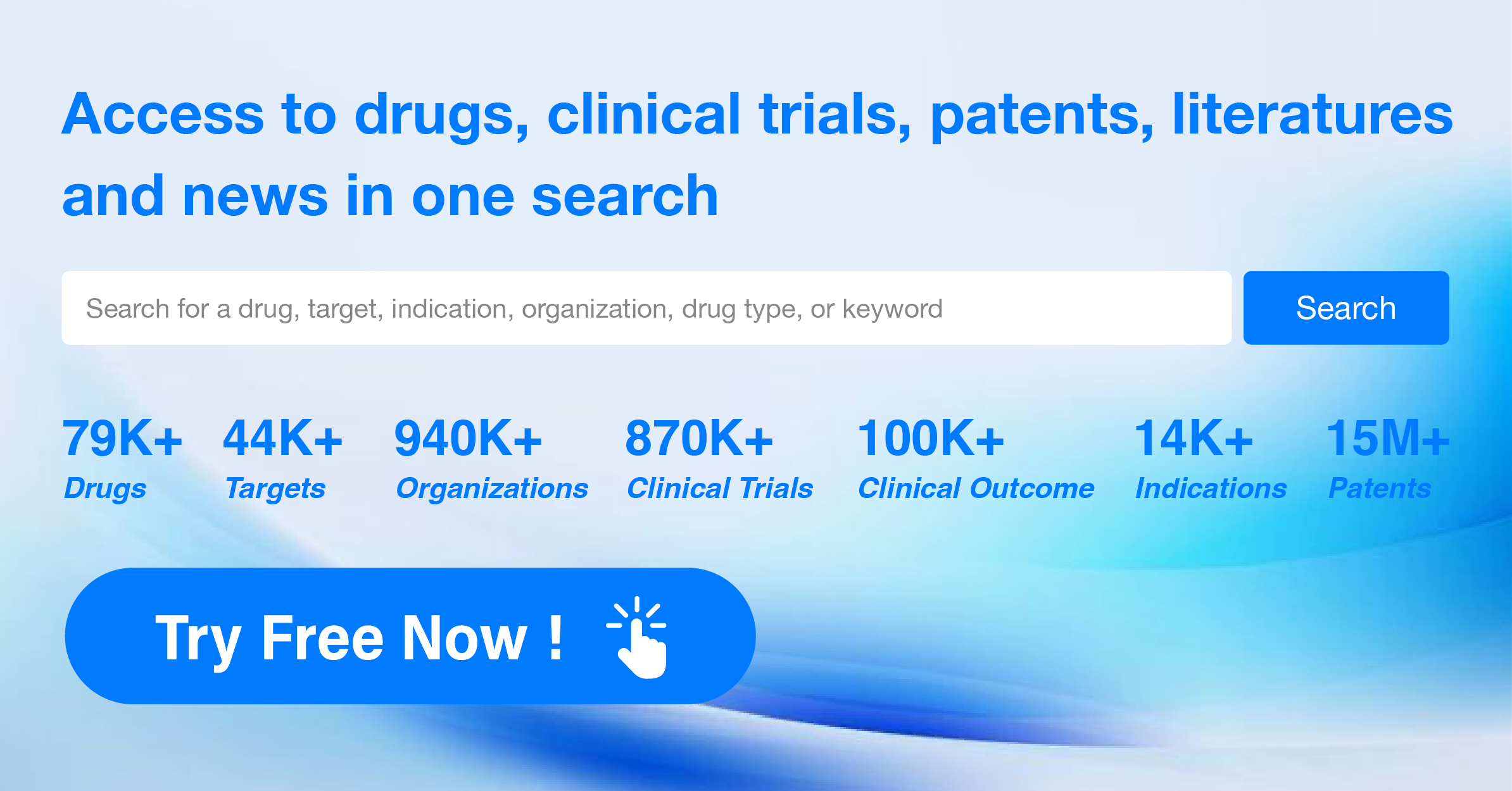
9.Clinical trials: Clinical trials provide valuable data on the safety and efficacy of new drug combinations. By conducting well-designed clinical trials, researchers can identify optimal dosage ranges for each drug in a combination based on its therapeutic effect and potential side effects.
10.Evidence-based medicine: When selecting drug combinations, it is crucial to consult scientific literature and guidelines from regulatory bodies. This approach ensures that the chosen combinations are supported by evidence and follow best practices.
In summary, optimizing drug dosage adjustments for individual patient profiles in the context of combination therapy requires a comprehensive understanding of various factors, including PK/PD, disease state, genetics, age, gender, organ impairment, drug interactions, and patient compliance. By considering these factors, healthcare providers can tailor drug treatments to maximize efficacy and minimize risks for each patient.