Request Demo
Last update 08 May 2025
Monkeypox(Asterivir)
Last update 08 May 2025
Overview
Basic Info
Drug Type Unknown |
Synonyms- |
Target- |
Action- |
Mechanism- |
Therapeutic Areas |
Active Indication |
Inactive Indication- |
Related
100 Clinical Results associated with Monkeypox(Asterivir)
Login to view more data
100 Translational Medicine associated with Monkeypox(Asterivir)
Login to view more data
100 Patents (Medical) associated with Monkeypox(Asterivir)
Login to view more data
119
Literatures (Medical) associated with Monkeypox(Asterivir)01 Mar 2025·European Journal of Internal Medicine
Oh no, all we needed was monkeypox!
Letter
Author: Lippi, Giuseppe
01 Mar 2025·STAR Protocols
Protocol for designing a peptide-based multi-epitope vaccine targeting monkeypox using reverse vaccine technology
Article
Author: Nagar, Garima ; Singh, Indrakant Kumar ; Mukherjee, Suprabhat ; Muduli, Rasmiranjan ; Kumar, Amit ; Kaur, Anupamjeet ; Chakraborty, Pritha ; Kundu, Rakesh ; Bhowmik, Prithwik ; Das, Mayami ; Majumdar, Tanmay ; Kumari, Geetika ; Shikha, Kumari
01 Jan 2025·Disaster Medicine and Public Health Preparedness
Smallpox Vaccines for Monkeypox: Is Emergency Vaccination Imminent?
Article
Author: Ahsan, Areeba ; E Mustafa Ahmed, Ghassan ; Tariq Ahmed, Samiuddin ; Abbasher Hussien Mohamed Ahmed, Khabab ; Mukareem Ali, Syed ; Fatima, Irtebaat ; Niaz, Faizan ; Waris, Abdul ; Ullah, Irfan
13
News (Medical) associated with Monkeypox(Asterivir)08 Mar 2023
MEXICO CITY--(
BUSINESS WIRE
)--Activists and public health experts in Mexico demand that officials of the Mexican Ministry of Health (SSA) and the Federal Commission for the Protection against Sanitary Risks (COFEPRIS) authorize the use of monkeypox (mpox) vaccines in the country.
"Despite the fact that mpox was declared a Public Health Emergency of International Concern by the World Health Organization (WHO) in July 2022, the vaccine recommended by the WHO to prevent infections is not yet authorized for use in Mexico," said Dr. Jorge Saavedra, Executive Director of the AHF Institute for Global Public Health, and one of the authors of the reply letter published in The Lancet Regional Health Americas. Dr. Saavedra added, “Strangely, Mexico is the only country in the top 10 with the most accumulated cases of mpox, which has not authorized the vaccine, as the other top nine have: USA, Brazil, Spain, UK, Colombia, Germany, France, Peru and Canada.”
In the current outbreak, mpox has disproportionately affected gay and bisexual men and severely affected those with advanced HIV, including cases that ended in death.
To deal with this health emergency, the WHO and the Centers for Disease Control have recommended the use of the vaccine for people at higher risk of exposure. The European Medicines Agency and the US FDA have also authorized the use of the vaccine.
Curiously, mpox vaccines were also recommended by officials of the Mexican Ministry of Health as a measure to contain the disease in a study published by the prestigious journal
The Lancet
. These officials, in their capacity as authors, correctly pointed out that the measures containment programs should, whenever available, include vaccines targeted at higher-risk groups. Among the authors of this study is the highest decision-maker in public health in Mexico, Dr. Hugo López-Gatell, Undersecretary of Health.
Dr. Gatell and the other authors of this study, which include Dr. Gustavo Reyes Terán (Head of the Coordinating Commission of National Institutes of Health and High Specialty Hospitals), Dr. Alethse de la Torre (General Director of the National AIDS Center-CENSIDA), who is in charge of HIV and STI policies and creating communication materials on mpox, as well as Dr. Gabriel García Rodríguez (General Director of Epidemiology) are the heads of the formulation of mpox policy in Mexico.
“It is disconcerting that Dr. López Gatell and these high level officials of the Ministry of Health, who are authors of this study, recommend the use of vaccines when addressing an international audience of health professionals through The Lancet, but they refuse to authorize any use of the mpox vaccine in their own country,” says Alain Pinzón of VIHve Libre, a local NGO that advocates for an effective response to HIV and
mpox
. “They say that there is not enough scientific evidence to authorize the vaccine, but they promoted the authorization in Mexico of the Chinese, Russian and Cuban vaccines against Covid-19, which had much less scientific evidence; so, for many of us, this not only sounds like hypocrisy, but institutional homophobia,” concluded Mr. Pinzón.
Human rights and public health activist Dr. Ricardo Baruch, another author of this letter, who has been pushing for the vaccine to be licensed since the beginning of this outbreak, says, “When we first read the article, we are very encouraged because high-level officials from the Mexican Ministry of Health expressed an opinion that was fully aligned with our advocacy efforts, as well as with the recommendations of the WHO, the EU and the CDC. However," he continues, "This was not what happened: Despite trying to raise awareness among officials in many ways, they have been reluctant to authorize its use."
After many unsuccessful attempts to convince Ministry of Health officials to follow the science and approve the use of mpox vaccines in Mexico, activists and public health professionals decided to write a reply to The Lancet to highlight the contradiction and express their concern. The letter was accepted and finally published by the same magazine in its correspondence section titled "
MPOX vaccines are needed in Mexico
,” on March 6, 2023. The authors of the letter highlight the discrepancy between words and actions and that, to date, mpox vaccines are not yet authorized for use by any person at serious risk in the country and they have not been purchased from the public sector either.
It has been demonstrated that vulnerable populations in Mexico need access to this vaccine that saves lives in the most serious cases and avoids unnecessary suffering in mild or not-so-serious cases. Currently, the only Mexicans who have been able to get vaccinated against mpox are those who have had money and/or a visa to travel to the United States, Canada, or Europe.
Mpox is a viral disease that was rarely seen outside of Africa until last year but has since affected more than 86,000 people in more than 110 countries and territories. Among the countries most impacted by the disease is Mexico, which has repeatedly been among the top ten countries, not only with the highest number of accumulated cases of mpox since the beginning of this outbreak, but also with the highest number of new cases in 2023.
AIDS Healthcare Foundation
(AHF) is a global non-profit organization providing cutting-edge medicine and advocacy to over 1.7 million people in 45 countries worldwide in the US, Africa, Latin America/Caribbean, the Asia/Pacific Region, and Europe. We are currently the largest non-profit provider of HIV/AIDS medical care in the world. To learn more about AHF, please visit our website:
www.aidshealth.org
, find us on Facebook:
www.facebook.com/aidshealth
and follow us on Twitter:
@aidshealthcare
and Instagram:
@aidshealthcare
.
Vaccine
20 Sep 2022
Monkeypox can sometimes lead to neurological complications such as encephalitis (brain inflammation), confusion or seizures, finds a new review of evidence.
Monkeypox can sometimes lead to neurological complications such as encephalitis (brain inflammation), confusion or seizures, finds a new review of evidence led by a UCL researcher.
Several studies incorporated in the systematic review and meta-analysis of evidence, published in eClinicalMedicine, also found that muscle aches, fatigue, headache, anxiety and depression were all relatively common among monkeypox patients.
Across the studies with relevant evidence, 2-3% of patients had severe complications such as seizure or encephalitis, although those studies mainly involved hospitalised patients from previous years. The researchers say there is not yet enough evidence to estimate neurological complication prevalence in the current outbreak.
The team led by researchers at UCL, Barts Health NHS Trust, Guy's and St Thomas' NHS Foundation Trust, and King's College London, looked for any studies reporting neurological or psychiatric symptoms of monkeypox that had been reported up until May 2022, before the outbreak spread globally.
Lead author Dr Jonathan Rogers (UCL Institute of Mental Health, UCL Psychiatry, and South London & Maudsley NHS Foundation Trust) said: "We found that severe neurological complications such as encephalitis and seizures, while rare, have been seen in enough monkeypox cases to warrant concern, so our study highlights a need for further investigation.
"There is also evidence that mood disorders such as depression and anxiety are relatively common for people with monkeypox."
Monkeypox primarily causes skin lesions and fever, and can be fatal, although in the current outbreak, substantially fewer than one in 1,000 confirmed cases have resulted in death. Although it has been endemic in parts of Central and West Africa for decades, with sporadic outbreaks elsewhere, 2022 has been the first time the virus has spread globally, attracting increased attention to an infectious disease that was previously relatively neglected.
The review incorporated 19 studies, with a total of 1,512 participants (1,031 of whom had a confirmed infection), in the US, Nigeria, Democratic Republic of Congo, Republic of Congo, and the UK.
By pooling data from across a sub-set of studies with relevant evidence, the researchers estimated that 2.7% of monkeypox patients experienced at least one seizure, 2.4% experienced confusion, and 2.0% had encephalitis, a serious condition of brain inflammation that can lead to long-term disability. There was very limited evidence for the prevalence of such symptoms, as the review only identified two cases of seizures, five cases of encephalitis and six cases of confusion (although other preliminary research has identified other cases), so larger studies are needed to better ascertain prevalence. The researchers say that further study is also needed to determine how monkeypox can impact the brain.
While the researchers were not able to pool data for psychosocial symptoms due to incomplete evidence, in some studies at least half of patients experienced at least one of myalgia (muscle aches), fatigue, headache, anxiety or depression. The researchers note that monkeypox may cause higher rates of mental ill health than other illnesses due to the presence of potentially disfiguring lesions, while there may also be stigma linked to how transmission is typically from close physical or sexual contact.
The studies reviewed did not have enough long-term follow-up with patients to know whether any of the symptoms last substantially longer than the acute phase of the illness. The researchers also caution that most cases in this review were hospitalised patients, and so the studied symptoms might not be as common in people with more mild cases.
Co-author Dr James Badenoch (Barts Health NHS Trust) said: "As there is still limited evidence into neurological and psychiatric symptoms in the current monkeypox outbreak, there is a need to set up coordinated surveillance for such symptoms.
"We suggest that clinicians should be watchful of psychiatric symptoms such as depression and anxiety and ensure that patients have access to psychological and psychiatric care if needed."
The study was funded by the Medical Research Council, Wellcome, and the NIHR University College London Hospitals Biomedical Research Centre, and involved researchers from UCL Psychiatry, UCL Queen Square Institute of Neurology, UCL Infection & Immunity, Barts, South London and Maudsley, Guy's and St Thomas', University College London Hospital, Queen Mary University of London, King's College London, the World Health Organization, and the Universities of Cambridge, Edinburgh, and Liverpool.
24 Aug 2022
Plume, a startup focused on virtual care for transgender patients, raised $24 million in Series B funding.
The round was led by Transformation Capital, with participation from General Catalyst and Town Hall Ventures. The investment comes about a year and half after the company announced a $14 million Series A.
WHAT IT DOES
Plume offers digital gender-affirming care, including prescriptions to hormone therapy like estrogen or testosterone, video consultations with providers, lab orders and analysis, support groups and medical letters of support for surgery or name and gender marker changes. In most states, the startup's membership costs $99 a month.
Plume plans to use the capital from the Series B to expand nationwide, move into virtual primary care and add insurance coverage for the company's services.
"With today's announcement, we are on track to reach our goal of increasing access to high-quality, gender-affirming care to patients across the U.S. in both urban areas and coverage deserts," Dr. Jerrica Kirkley, Plume cofounder and chief medical officer, said in a statement.
"Knowing the hurdles trans Americans face when accessing care, I'm encouraged to reach this benchmark and I look forward to Plume's growth in the future. I want to thank Transformation Capital, General Catalyst, and Town Hall Ventures for their partnership in transforming health care for every trans life."
MARKET SNAPSHOT
Another digital health company working with LGBTQIA+ patients is Folx Health, which announced a $25 million Series A raise in February 2021. Folx recently launched an employer offering and added counseling, evaluation and referrals for Monkeypox treatment.
Last year, the recently merged virtual care companies Grand Rounds Health and Doctor On Demand acquired Included Health, a health concierge platform for the LGBTQIA+ community. The company later rebranded under the Included name.
Like a number of other digital health and health tech companies pursuing layoffs this summer, Included recently reduced its workforce by less than 6% as part of a company restructuring.
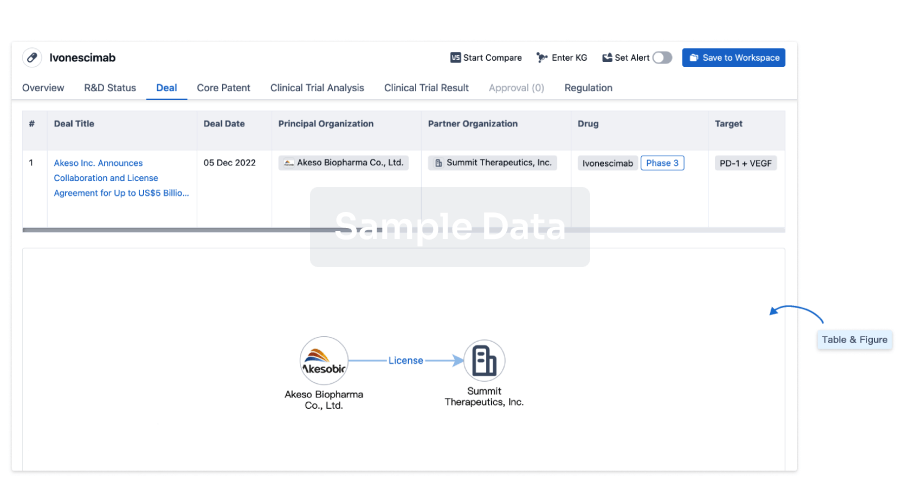
100 Deals associated with Monkeypox(Asterivir)
Login to view more data
R&D Status
10 top R&D records. to view more data
Login
| Indication | Highest Phase | Country/Location | Organization | Date |
|---|---|---|---|---|
| Monkeypox | Preclinical | Switzerland | 07 May 2024 |
Login to view more data
Clinical Result
Clinical Result
Indication
Phase
Evaluation
View All Results
| Study | Phase | Population | Analyzed Enrollment | Group | Results | Evaluation | Publication Date |
|---|
No Data | |||||||
Login to view more data
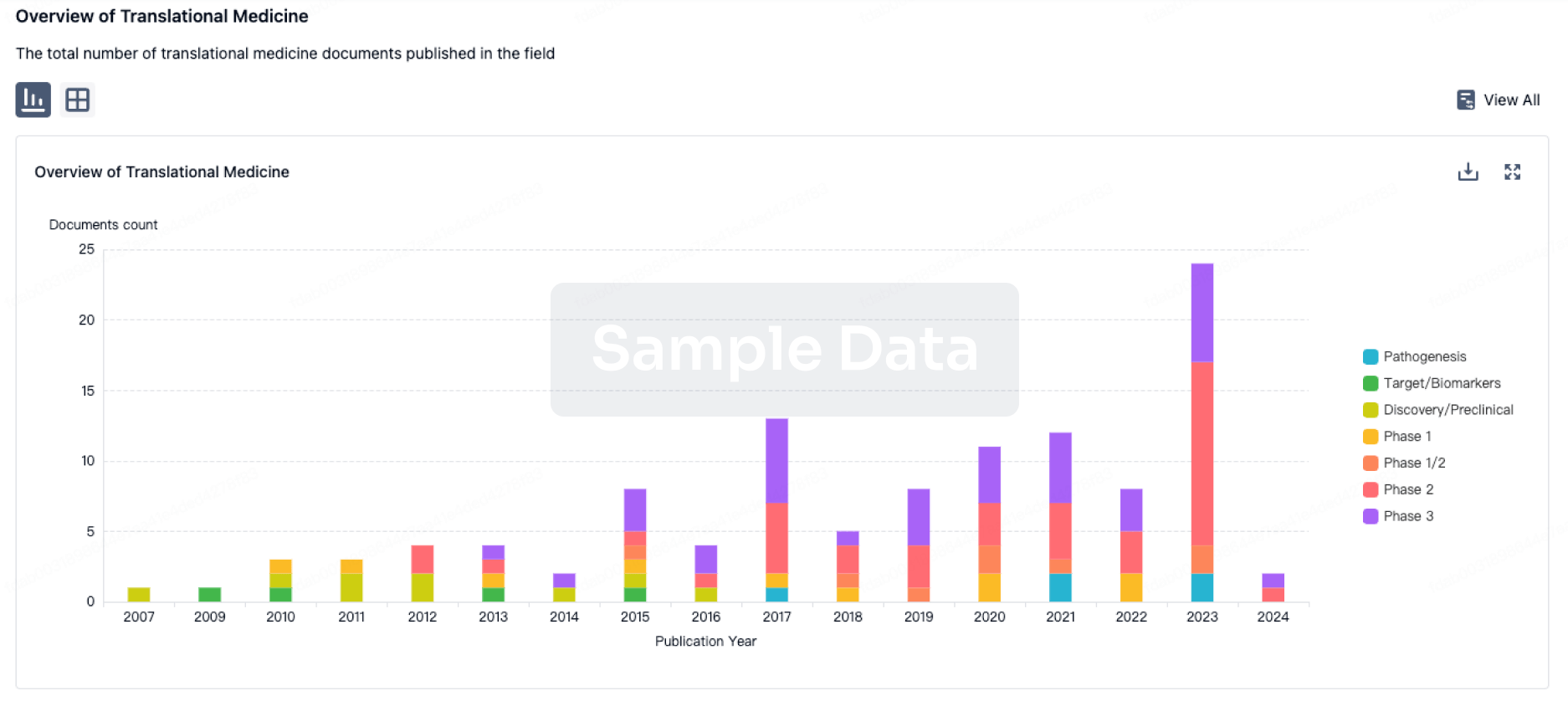
Translational Medicine
Boost your research with our translational medicine data.
login
or
Deal
Boost your decision using our deal data.
login
or
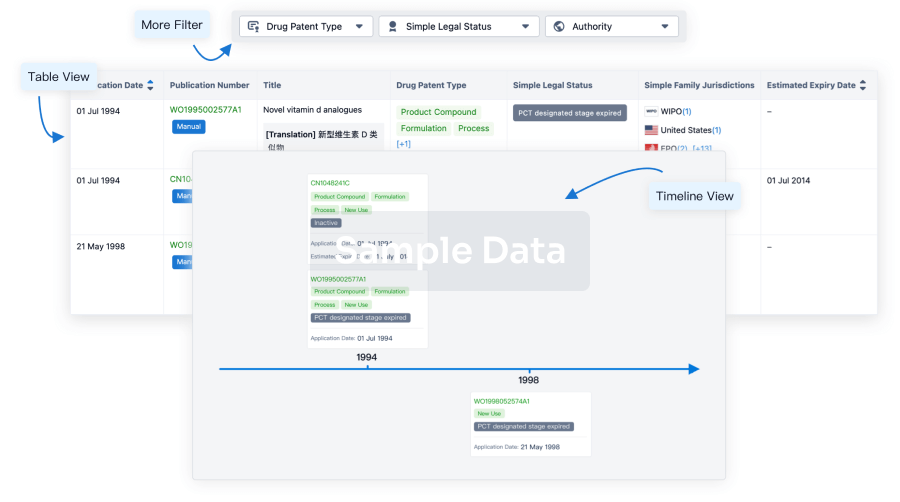
Core Patent
Boost your research with our Core Patent data.
login
or
Clinical Trial
Identify the latest clinical trials across global registries.
login
or
Approval
Accelerate your research with the latest regulatory approval information.
login
or

Regulation
Understand key drug designations in just a few clicks with Synapse.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free
