Request Demo
Last update 23 Jan 2025
Low-molecular-weight heparin
Last update 23 Jan 2025
Overview
Basic Info
Drug Type Chemical drugs |
Synonyms LMWH |
Target- |
Mechanism- |
Active Indication |
Inactive Indication- |
Originator Organization- |
Inactive Organization- |
Drug Highest PhasePreclinical |
First Approval Date- |
Regulation- |
Related
18
Clinical Trials associated with Low-molecular-weight heparinNCT06729021
Predictive Efficacy of Modified Caprini Score and D-Dimer for the Evaluation and Management of Lower Extremity Venous Thrombosis Among Cardiothoracic Surgery Patients in Baghdad
The goal of this observational study is to evaluate the predictive efficacy of the Modified Caprini Risk Assessment Score and D-Dimer in identifying and managing lower extremity venous thrombosis (LEVT) among cardiothoracic surgery patients in Baghdad. The main questions it aims to answer are:
Does combining the Modified Caprini Score with D-Dimer improve the accuracy of predicting lower extremity venous thrombosis (LEVT) compared to using each tool independently? Can these tools effectively guide clinical decisions for lower extremity venous thrombosis (LEVT) prevention and management in this patient population?
Participants will:
Undergo risk assessment for lower extremity venous thrombosis (LEVT) using the Modified Caprini Score and have their D-Dimer levels measured during their hospital stay.
Be monitored for clinical outcomes, including confirmed lower extremity venous thrombosis (LEVT) incidence, need for anticoagulation therapy, and complications such as pulmonary embolism or recurrent thrombosis.
Does combining the Modified Caprini Score with D-Dimer improve the accuracy of predicting lower extremity venous thrombosis (LEVT) compared to using each tool independently? Can these tools effectively guide clinical decisions for lower extremity venous thrombosis (LEVT) prevention and management in this patient population?
Participants will:
Undergo risk assessment for lower extremity venous thrombosis (LEVT) using the Modified Caprini Score and have their D-Dimer levels measured during their hospital stay.
Be monitored for clinical outcomes, including confirmed lower extremity venous thrombosis (LEVT) incidence, need for anticoagulation therapy, and complications such as pulmonary embolism or recurrent thrombosis.
Start Date20 Dec 2024 |
Sponsor / Collaborator |
NCT05512702
Treatment Approach in Patients Diagnosed With Pulmonary Thromboembolism With Intermediate-High Risk Interms of Early Mortality After the Establisment of Ege Pulmonary Embolism Team
Pulmonary Embolism(PE) requires multidisciplinary approach as a highly morbid and mortal disease. This multidisciplinary approach creates clinical benefits in diagnostic and therapeutic process. And these benefits are pointed out in certain studies and guidelines. For these reasons, a Pulmonary Embolism Response Team (PERT) was established on 5 th November 2018 which is called as Ege Pulmonary Embolism Team (EGEPET) in our university.
In recent years, it is stated that the carefully use of thrombolytic in patients with intermediate-high risk PE based on early mortality classification. Some studies have reported that the use of thrombolytic may cause clinical benefits. But which used drug and which dose are not defined clearly yet.
After establishment of EGEPET, the investigators observed that patients with intermediate-high risk PE more receive reduced dose thrombolytic than the pre-EGEPET period. And the investigators aimed to compare treatment changes after and before the establishment of EGEPET. Also, the investigator will compare initial reduced dose thrombolytic therapy after EGEPET with initial anticoagulation therapy before EGEPET (historical group) in terms of mortality and complication.
As the reduced dose thrombolytic, Alteplase 50 mg is used in our hospital. Low-molecular weight heparin (LMWH), standard heparin and rarely Fondaparinux are used for anticoagulation therapy. Low-molecular weight heparin is generally applied for treatment, in case there is no contraindication.
Our primary end-point is to assess 30-day mortality and secondary-end points are to detect in one year-mortality and complications. The investigators will compare the mortality and complication rates in these groups.
N0 hypothesis; In the intermediate-high risk group diagnosed with PE, there is an increased mortality rate in the patients treated with half-dose thrombolytic (Alteplase 50 mg) than our historical group or the literature.
N1 hypothesis; In the intermediate-high risk group diagnosed with PE, there is no an increased mortality rate in the patients treated with half-dose thrombolytic (Alteplase 50 mg) than our historical group or the literature.
In recent years, it is stated that the carefully use of thrombolytic in patients with intermediate-high risk PE based on early mortality classification. Some studies have reported that the use of thrombolytic may cause clinical benefits. But which used drug and which dose are not defined clearly yet.
After establishment of EGEPET, the investigators observed that patients with intermediate-high risk PE more receive reduced dose thrombolytic than the pre-EGEPET period. And the investigators aimed to compare treatment changes after and before the establishment of EGEPET. Also, the investigator will compare initial reduced dose thrombolytic therapy after EGEPET with initial anticoagulation therapy before EGEPET (historical group) in terms of mortality and complication.
As the reduced dose thrombolytic, Alteplase 50 mg is used in our hospital. Low-molecular weight heparin (LMWH), standard heparin and rarely Fondaparinux are used for anticoagulation therapy. Low-molecular weight heparin is generally applied for treatment, in case there is no contraindication.
Our primary end-point is to assess 30-day mortality and secondary-end points are to detect in one year-mortality and complications. The investigators will compare the mortality and complication rates in these groups.
N0 hypothesis; In the intermediate-high risk group diagnosed with PE, there is an increased mortality rate in the patients treated with half-dose thrombolytic (Alteplase 50 mg) than our historical group or the literature.
N1 hypothesis; In the intermediate-high risk group diagnosed with PE, there is no an increased mortality rate in the patients treated with half-dose thrombolytic (Alteplase 50 mg) than our historical group or the literature.
Start Date03 Jun 2022 |
Sponsor / Collaborator |
NL-OMON28133
Intranasal LMWH against COVID-19
Start Date20 Jan 2021 |
Sponsor / Collaborator |
100 Clinical Results associated with Low-molecular-weight heparin
Login to view more data
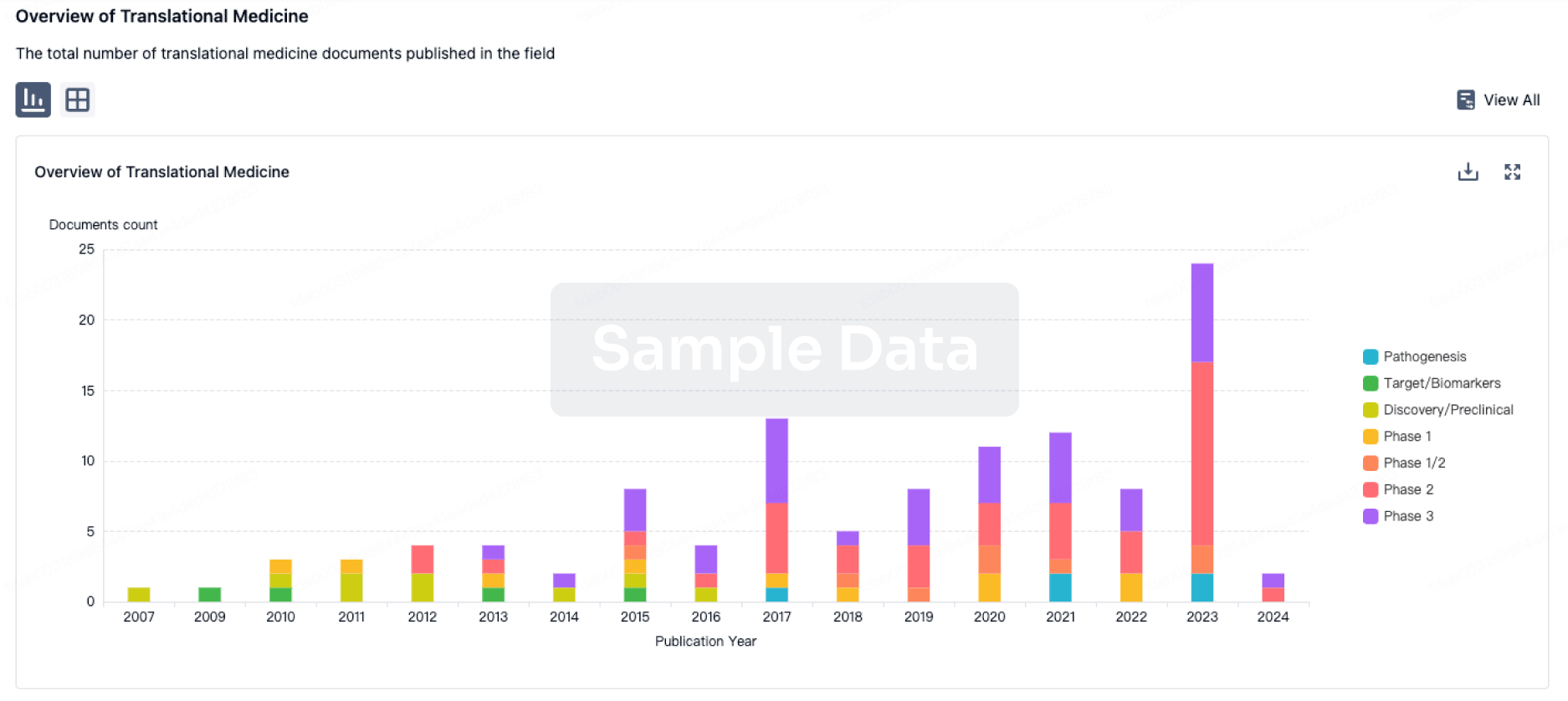
100 Translational Medicine associated with Low-molecular-weight heparin
Login to view more data
100 Patents (Medical) associated with Low-molecular-weight heparin
Login to view more data
371
Literatures (Medical) associated with Low-molecular-weight heparin01 Apr 2025·Journal of Critical Care
A retrospective Cohort study on the effect of the LOw-molecular weighT heparin (LMWH) nadroparin dose on anti-XA levels in a mixed medical-surgical ICU population: CLOT-Xa
Article
Author: van Berkel, Lisanne ; Adriaansen, Henk J ; Hulstein, Janine J J ; Spronk, Peter E ; Kuindersma, Marnix ; van Iperen, Ingrid D
01 Mar 2025·International Journal of Biological Macromolecules
Low-molecular-weight heparin sodium inhibits the MAPK pathway for psoriasis treatment in mice
Article
Author: Wang, Jing ; Zhang, Zhenhai ; Shu, Luan ; Fang, Zhijun ; He, Chen ; Guo, Yanyan ; Zhong, Ziyi
01 Feb 2025·Head & Neck
Effect of Low Molecular Weight Heparin Calcium on Prevention of Lower Limb Deep Venous Thrombosis in Oral Cancer Patients With Anterolateral Thigh Flap Reconstruction
Article
Author: Wu, Kun ; Lu, Linsong ; Zhi, Yuan ; Gong, Zhaojian ; Zi, Moxin ; Zhang, Xiangyu ; Liu, Keyue
2
News (Medical) associated with Low-molecular-weight heparin06 Jun 2023
TUESDAY, June 6, 2023 -- Direct oral anticoagulant (DOAC) treatment is noninferior to low-molecular-weight
heparin
(LMWH) for preventing recurrent
venous thromboembolism
(VTE) in cancer patients, according to a study published online June 2 in the
Journal of the American Medical Association
to coincide with the annual meeting of the American Society of Clinical Oncology, held from June 2 to 6 in Chicago.
Deborah Schrag, M.D., from the Memorial Sloan Kettering Cancer Center in New York City, and colleagues assessed the effectiveness of DOACs (335 patients) versus LMWH (336 patients) for preventing recurrent VTE in patients with cancer (any invasive solid tumor, lymphoma, multiple myeloma, or chronic lymphocytic leukemia) over six months.
The researchers found that rates of recurrent VTE were 6.1 percent in the DOAC group versus 8.8 percent in the LMWH group (difference, −2.7 percent), consistent with the prespecified noninferiority criterion. None of the six prespecified secondary outcomes were significantly different between the groups. Major bleeding did not meet the noninferiority criterion, as it occurred in 5.2 percent of the DOAC group versus 5.6 percent of the LMWH group (difference, −0.4 percent; 1-sided 95 percent confidence interval, –100 percent to 2.5 percent). Severe adverse events occurred in 33.8 percent and 35.1 percent of the groups, respectively. Anemia and death were the most common serious adverse events reported.
"These findings support use of a DOAC to prevent recurrent VTE in patients with cancer," the authors write.
Several authors disclosed ties to the pharmaceutical industry.
Abstract/Full Text
More Information
Posted June 2023
Clinical ResultASCO
23 Aug 2021
In a presentation at ESC Congress 2021, world-renowned blood clot expert Alex C. Spyropoulos reveals clinical trial data
MANHASSET, N.Y.--(BUSINESS WIRE)-- Throughout the pandemic, the medical community witnessed an increased risk for major blood clotting and death in patients with coronavirus disease 2019 (COVID-19). The Feinstein Institutes for Medical Research’s Alex C. Spyropoulos, MD, will reveal during a “Latest Science” presentation at ESC Congress 2021, organized by the European Society of Cardiology (ESC) clinical trial results that show significant improvement at preventing these clots.
This press release features multimedia. View the full release here:
Alex Spyropoulos, MD, the trial’s principal investigator and professor at Feinstein Institutes’ Institute of Health System Science. (Credit: The Feinstein Institutes for Medical Research)
Dr. Spyropoulos’ HEP-COVID clinical trial revealed that prophylaxis with therapeutic low-dose heparin significantly reduces major thromboembolism (clotting) and death in high-risk hospitalized patients versus standard-of-care thromboprophylaxis. Results found that the incidence of major thromboembolism and death in patients was 28.7 percent for those given a therapeutic-dose low-molecular-weight heparin (LMWH) versus 41.9 percent for those who received institutional standard prophylactic or intermediate-dose heparins.
Since May 2020, Dr. Spyropoulos and his team enrolled 257 critically sick hospitalized adults in a randomized controlled multi-center clinical trial, HEP-COVID, to determine which dosage of heparin – an anticoagulation medication – is most effective.
“In the HEP-COVID clinical trial we were able to predict a population of hospitalized COVID-19 that are at high risk of developing thromboembolic complications and death and alter their outcomes with a therapeutic dose of heparin, without major bleeding,” said Dr. Spyropoulos, the trial’s principal investigator and professor at Feinstein Institutes’ Institute of Health System Science. “We hope that our findings will inform others clinicians on the frontlines on the most effective weapon we have to prevent these often morbid and fatal thrombotic complications from COVID-19.”
The therapeutic dose of heparin was four times that of the standard dose and patients were assessed for their risk using a relatively new elevated blood biomarker test, the D-dimer. Treatment results were not seen in patients who were critically ill requiring ICU level of care – indicating that by assessing patient risk prior to intensive care and delivering LMWH clinicians could alter the course of disease. This shift in medication dosage may result in health systems revising the current standard of care procedures for preventing thrombotic complications in high-risk COVID-19 hospitalized patients.
Dr. Spyropoulos is system director of Anticoagulation and Clinical Thrombosis Services at Northwell Health, has been on the forefront of studying thrombotic complications in COVID-19 patients in the outpatient setting, during hospitalization, and the post hospital discharge period to assess their risk and best treatments. Most recently, in research published in the journal Blood, his team identified those COVID-19 patients post-discharge at high-risk of thrombotic complications and death and determined that post-discharge anticoagulants – mostly at prophylactic dosages – reduce the risk of major thromboembolic events and death by 46 percent.
“Blood clots cause serious complications for patients with COVID-19 in the hospital and at home,” said Kevin J. Tracey, MD, president and CEO of the Feinstein Institutes. “Dr. Spyropoulos is a leader in studying and understanding these complications. The HEP-COVID clinical trial results are a new milestone to guide advances in care.”
At the start of the pandemic, the Feinstein Institutes pivoted to focus clinical trials to study the efficacy and safety of therapeutics to treat those with the virus. Since Feinstein Institutes’ COVID-19 Clinical Trial Unit was formed in March 2020, 15 clinical trials were initiated and enrolled more than 1,700 patients, including patients for the HEP-COVID trial.
Additionally, this study was published through the Northwell Health Research Consortium which began in early 2020 and has organized more than 500 clinicians, statisticians and scientists across the Feinstein Institutes and Northwell Health to conduct cutting-edge research about the COVID-19 pandemic. To date, more than 500 manuscripts have been written addressing the most pressing questions surrounding the virus.
About the Feinstein Institutes
The Feinstein Institutes for Medical Research is the research arm of Northwell Health, the largest health care provider and private employer in New York State. Home to 50 research labs, 2,500 clinical research studies and 5,000 researchers and staff, the Feinstein Institutes raises the standard of medical innovation through its five institutes of behavioral science, bioelectronic medicine, cancer, health innovations and outcomes, and molecular medicine. We make breakthroughs in genetics, oncology, brain research, mental health, autoimmunity, and are the global scientific leader in bioelectronic medicine – a new field of science that has the potential to revolutionize medicine. For more information about how we produce knowledge to cure disease, visit feinstein.northwell.edu.
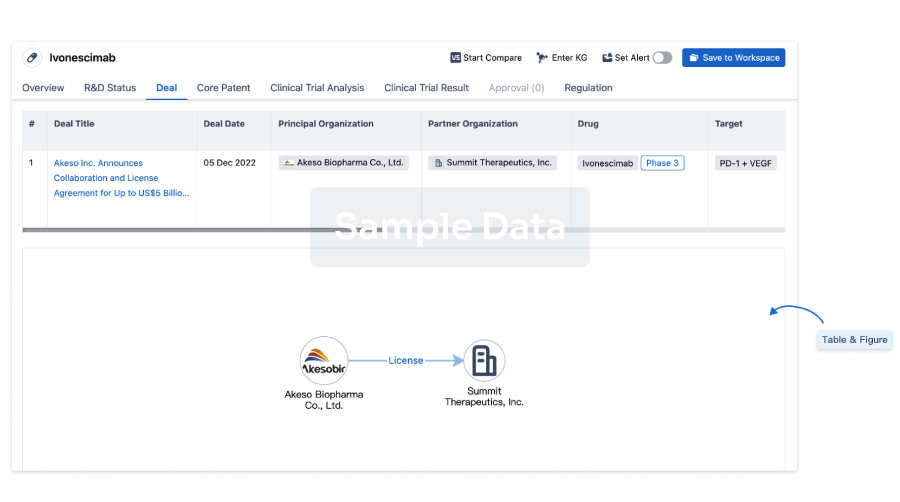
100 Deals associated with Low-molecular-weight heparin
Login to view more data
R&D Status
10 top R&D records. to view more data
Login
| Indication | Highest Phase | Country/Location | Organization | Date |
|---|---|---|---|---|
| Inflammatory Bowel Diseases | Preclinical | CN | 06 Jul 2024 | |
| Thrombosis | Preclinical | GB | 24 Jun 2023 | |
| Thrombosis | Preclinical | GB | 24 Jun 2023 |
Login to view more data
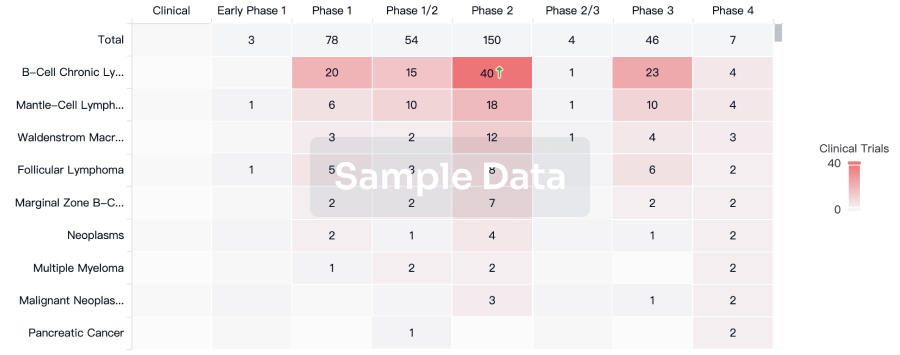
Clinical Result
Clinical Result
Indication
Phase
Evaluation
View All Results
| Study | Phase | Population | Analyzed Enrollment | Group | Results | Evaluation | Publication Date |
|---|
No Data | |||||||
Login to view more data
Translational Medicine
Boost your research with our translational medicine data.
login
or
Deal
Boost your decision using our deal data.
login
or
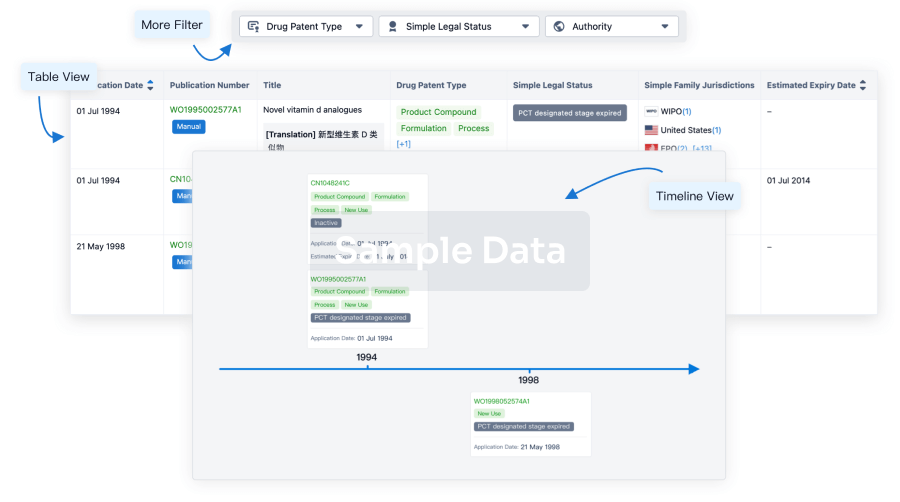
Core Patent
Boost your research with our Core Patent data.
login
or
Clinical Trial
Identify the latest clinical trials across global registries.
login
or
Approval
Accelerate your research with the latest regulatory approval information.
login
or
Regulation
Understand key drug designations in just a few clicks with Synapse.
login
or
Chat with Hiro
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free





