Impact of the BOOST GAIT Program on Gait Recovery and Functional Mobility After Stroke - a Pilot Study Impact Van Het BOOST GAIT Programma Op Het Herstel Van Het Gangbeeld En Functionele Mobiliteit Na Een Beroerte - Een Pilootstudie
The overarching goal is to determine if the BOOST GAIT program can improve functional mobility in patients with stroke who are undergoing inpatient rehabilitation and have some walking function, through the application of augmented therapeutic exercises designed to achieve a normative gait pattern. The evaluation will be conducted using a combination of clinical scales and objective motion sensors that map walking quality and performance during activities of daily living, such as rising from a chair and standing.
It is acknowledged that this single-group pilot study, which aims to include 12 participants, is insufficiently powered to address the primary objective. A larger parallel-design study is required to definitively address this issue. To help design a larger study, the current objectives are: first, to have realistic expectations regarding recruitment and dropout rates; second, to identify potential barriers to therapy adherence and data collection that may impede the success of a larger study; third, assess the test-retest reliability of sensor-based motion capture of movement quality during walking and related tasks in hemiparetic stroke patients. For the latter objective, the sensor measurements at the end of the intervention will be repeated on two consecutive days.
In addition to their usual care, participants will undergo additional therapy over a four-week period, with sessions occurring five times per week for one hour as part of the BOOST GAIT program. The BOOST GAIT sessions will be conducted as group-based therapy with four patients and two physiotherapists present to oversee the performance of mobility-specific exercises, including sit-to-stand transfers, standing and stepping, and eventually walking. The rationale for this approach is that the combined effects of augmenting the amount of therapeutic exercises and specifically targeting motor control of the paretic leg will facilitate symmetry during tasks, which in turn will have carry-over effects on safe performance of walking and other mobility tasks.
Targeting Fear of Cancer Recurrence in Cancer Survivors: a Multicentre Randomized Controlled Trial to Evaluate Internet-Based Emotional Freedom Techniques and Internet-Based Mindfulness Meditation as Intervention Strategies
In this trial, the investigators introduce two internet-based psychological methods to meet the currently unmet medical need to cope with Fear of Cancer Recurrence (FCR) beyond the acute phase of cancer treatment: internet-based emotional freedom techniques (iEFT) and internet-based mindfulness intervention (iMMI). The primary aim of this trial is to examine the efficacy of Internet-Based Emotional Freedom Techniques (iEFT) and Internet-Based Mindfulness Meditation Intervention (iMMI) to alleviate Fear of Cancer Recurrence (FCR) in cancer survivors, as determined through the Fear of Cancer Recurrence Inventory (FCRI) in cancer survivors. To translate a statistically significant effect on FCR into a clinically significant change, the investigators would need to detect a between-group difference in mean FCRI at T1 of 10 points using an independent samples t-test (two experimental groups are compared against a single wait-list control). When the application of iEFT and/or iMMI appears effective to reduce FCR, these self-help methods could be implemented in clinical settings. The use of these low cost interventions with a low threshold, by an internet-based approach, will facilitate a potential implementation in clinical practice.
Aha BOOST Arm-hand BOOST Therapy to Enhance Recovery After Stroke: Clinical, Health Economic and Process Evaluation
The overall aim of this study is to establish the clinical- and cost-effectiveness of the arm-hand BOOST therapy when delivered on top of the usual care program in the sub-acute phase post stroke and to perform a process evaluation.
In this phase III RCT, 80 patients with stroke will be recruited from two inpatient stroke rehabilitation wards in Belgium and randomized to the experimental group receiving arm-hand BOOST therapy or the control group receiving the L-BOOST intervention, on top of their usual inpatient care program. The arm-hand BOOST program (1 hour/day, 5x/week, 4 weeks) consists of group exercises based on four key aspects, namely neurophysiology, sequences of reaching and grasping, de-weighting of the arm, and orientation of the hand towards objects. Additionally, technology-supported upper limb therapy will be provided two times 30 minutes per week. The L-BOOST intervention comprises a dose-matched program of lower limb exercises and general reconditioning. At baseline, after 4 weeks of training, 3 months after the intervention and at 12 months post stroke, outcome assessment will be performed. The primary outcome measure is the action research arm test (ARAT). Secondary outcomes include measures in the domain of upper limb function and capacity, independence, participation and quality of life. Multivariate ANOVA and sensitivity analyses will be used to compare change from baseline between groups. Information on medical costs will be collected to allow a health economic evaluation. Finally, a process evaluation will be performed to assist in identifying why arm-hand BOOST succeeds or fails unexpectedly or has unanticipated consequences, and how this can be optimized.
At the start of this study the investigators hypothesize that: (I) Aha BOOST will result in a significant greater improvement in arm-hand activity post-intervention, at follow-up and 12 months post stroke compared to control therapy (L-BOOST); (II) Aha BOOST will result in a significant greater improvement in upper limb function, performance, independence and activity of daily living, and participation post-intervention, at follow up and 12 months post stroke. (III) Investing in 24 hours of extra arm-hand therapy to subacute stroke patient in the inpatient rehabilitation setting can reduce the health-economic and societal cost 12 months post stroke.
100 Clinical Results associated with Fortis Jessa Ram Hospital
0 Patents (Medical) associated with Fortis Jessa Ram Hospital
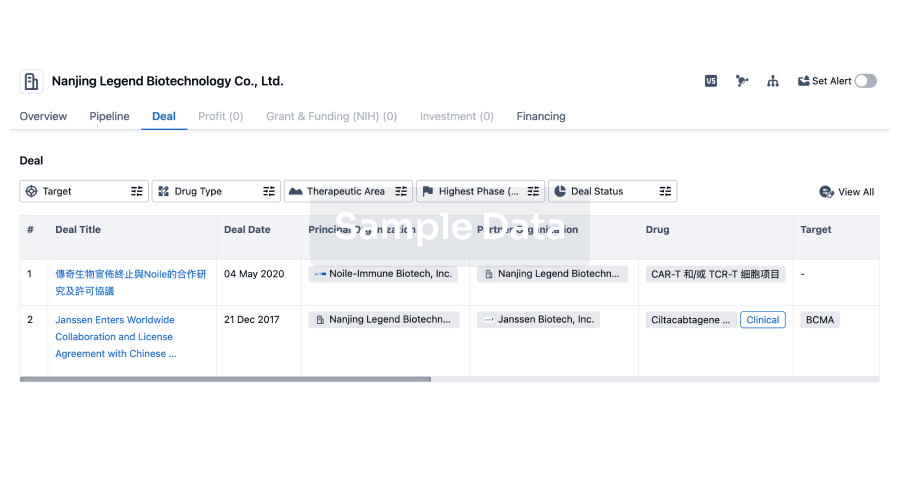
100 Deals associated with Fortis Jessa Ram Hospital
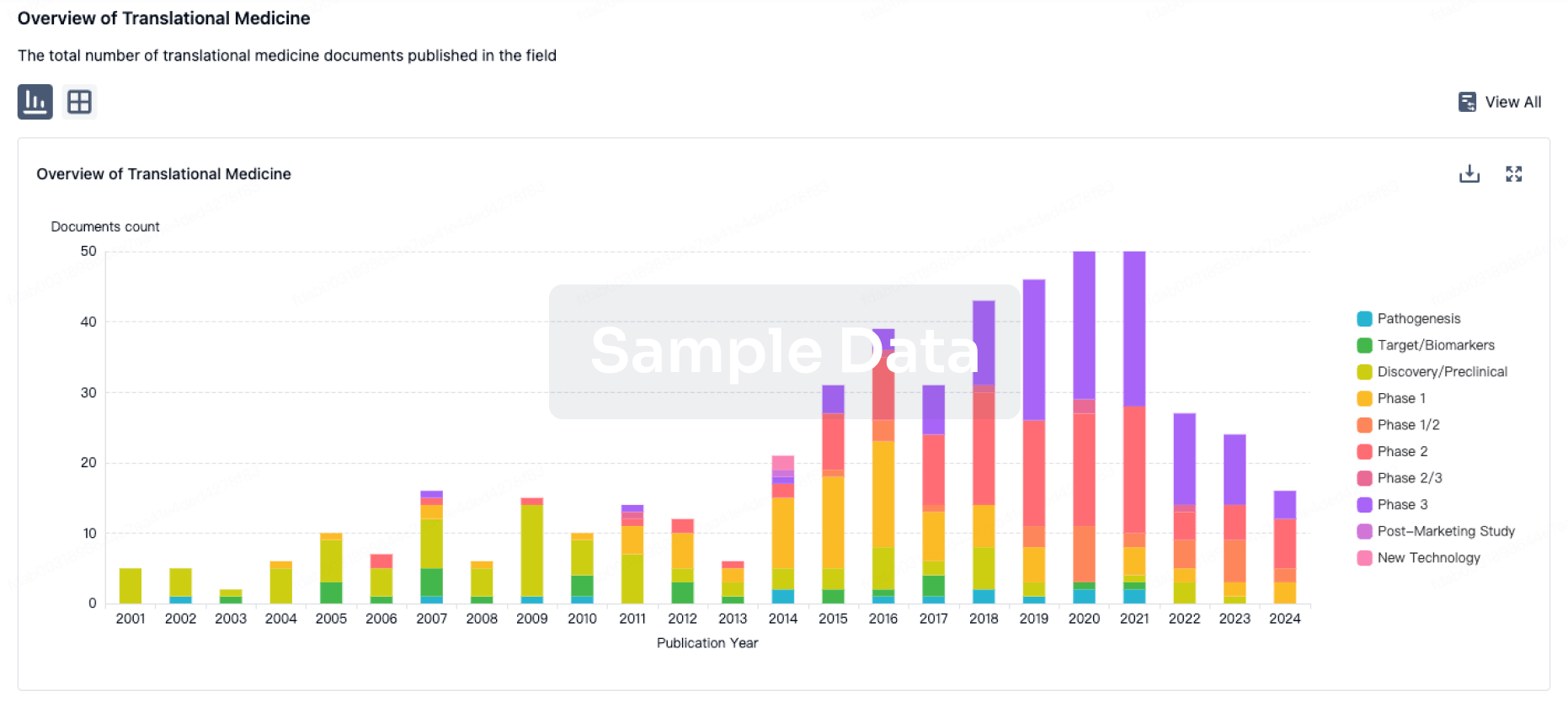
100 Translational Medicine associated with Fortis Jessa Ram Hospital