Request Demo
Last update 08 May 2025

University of Minnesota College of Pharmacy
Last update 08 May 2025
Overview
Related
100 Clinical Results associated with University of Minnesota College of Pharmacy
Login to view more data
0 Patents (Medical) associated with University of Minnesota College of Pharmacy
Login to view more data
465
Literatures (Medical) associated with University of Minnesota College of Pharmacy01 May 2025·Currents in Pharmacy Teaching and Learning
Exploring the unanticipated value of an oral exam integrating content across courses
Article
Author: Janke, Kristin K ; Lepp, Gardner A ; Westberg, Sarah M ; Lee, Jungeun
01 Apr 2025·JACC: CardioOncology
Long-Term Care of Childhood Cancer Survivors at Risk for Cardiac Late Effects
Author: Narasimhan, Shanti ; Ly, Daniel ; Dabour, Mohamed S ; Ackerman, Aaron ; Sadak, Karim T ; Elsherif, Mahmoud ; Rodgers, Nathan ; Zordoky, Beshay N ; Hall, Monica
01 Apr 2025·International Journal of Infectious Diseases
Beyond the guidelines: original research on real-world outcomes of anticoagulation and corticosteroid in COVID-19
Article
Author: Tessier, Katelyn M ; Hozayen, Sameh ; Chapman, Scott A ; Tignanelli, Christopher ; Leslie, Alison
10
News (Medical) associated with University of Minnesota College of Pharmacy07 Jan 2025
WAKEFIELD, Mass.--(
BUSINESS WIRE
)--
The Health System Owned Specialty Pharmacy Alliance (HOSP)
is pleased to announce the appointment of Tim Affeldt, PharmD, Vice President, Specialty/Infusion Operations, Fairview Pharmacy Services, as its new President. Dr. Affeldt brings a wealth of experience and a passion for advancing the specialty pharmacy field, positioning HOSP for continued growth and impact in the healthcare sector.
“I am confident that Tim will build on our strong foundation and lead the organization to even greater achievements. His vision and expertise will be invaluable as HOSP continues to advocate for the critical role of health system-owned specialty pharmacies in improving patient care,” said President Emeritus Gary Kerr.
Dr. Affeldt has been a key figure in shaping HOSP’s mission and strategic direction. A graduate of the University of Minnesota, College of Pharmacy, Dr. Affeldt joined Fairview Pharmacy Services in 2013, where he has provided strategic leadership to various pharmacy services, including Specialty and Mail Order pharmacies, Infusion Center pharmacy, and Home Infusion. In addition to his role at Fairview, Dr. Affeldt has served as Treasurer of HOSP and contributed to numerous professional organizations, including the National Home Infusion Association and the National Association of Specialty Pharmacy.
Dr. Affeldt shared his excitement about the opportunity to lead HOSP. “I am thrilled to take on this role and continue the exceptional work that Gary and the HOSP team have accomplished. Together, we will work to address the challenges facing health system-owned specialty pharmacies and seize new opportunities to enhance patient outcomes and advance our profession,” said Dr. Affeldt. “We thank Gary for his outstanding contributions and leadership during his tenure.”
About HOSP:
The Health System Owned Specialty Pharmacy Alliance (HOSP) is a network of leading health systems and supporting businesses dedicated to advocating for superior patient care and outcomes through fully integrated health system specialty pharmacies. HOSP believes that health systems are best positioned to deliver the highest quality care to specialty patients in the outpatient setting. For more information, visit
https://hospalliance.org/
.
Executive Change
12 Dec 2024
WASHINGTON, Dec. 12, 2024 /PRNewswire/ -- Today, the American Pharmacists Association (APhA) began announcing the selection of the 2025 APhA Awards and Honors Program recipients. The APhA Awards and Honors Program is the most comprehensive recognition program in the profession of pharmacy. All honorees in the profession-wide, practitioner, research, and student pharmacist categories will be announced over the next few weeks and can be found on APhA's
awards website. Recipients will be officially recognized during the
APhA Annual Meeting & Exposition in Nashville, TN, March 21–24, 2025.
The Remington Honor Medal was named for eminent community pharmacist, manufacturer, and educator, Joseph P. Remington and was established in 1918 to recognize distinguished service on behalf of American pharmacy during the preceding years that culminate in the past year or during a long period of outstanding activity or fruitful achievement. It serves as the preeminent award for the profession of pharmacy and is the highest honor bestowed by APhA.
Stephen W. Schondelmeyer, PharmD, PhD, of Minneapolis, MN, was selected as the recipient of the 2025 Remington Honor Medal. Schondelmeyer's impact and expertise from over 50 years of research includes improving prescription drug access and affordability, encouraging drug price competition, shaping drug benefit plan management and prescription drug reimbursement, documenting pharmacists' compensation and workforce trends, and establishing policy to reduce drug shortages and improve drug supply resilience.
His work experience has encompassed activities in practice, academia, professional associations, and state and federal government. Dr. Schondelmeyer is currently a professor of Pharmaceutical Economics in the College of Pharmacy at the University of Minnesota where he holds the Century Mortar Club Endowed Chair in Pharmaceutical Management & Economics. Dr. Schondelmeyer established and is Director of the PRIME Institute at the University of Minnesota, which conducts economic and public policy research on the roles of pharmacists and pharmaceuticals in society.
Schondelmeyer's nominators note that "his work has shaped medication and health policy as we know it today." One nominator highlighted Schondelmeyer's broad efforts to share "who pharmacists are" and "how they can improve the distribution and use of medications in society" to those outside of the pharmacy profession, which has greatly increased public visibility on the value of pharmacists.
Another nominator noted his contribution to the body of knowledge and efforts to share this knowledge broadly are unmatched with 930 invited presentations, 260 scientific peer reviewed papers, posters, and presentations, 174 technical reports, books, and book chapters about drug pricing, supply chain management, drug shortages, and pharmacy policy, and 160 presentations and testimony to Congress, state legislatures, and other governmental entities.
In addition to his own research endeavors, Schondelmeyer has served as an expert on numerous state and national task forces and boards where he shares the value of pharmacy and improves patient lives through policy. Schondelmeyer has received numerous awards and honors, including APhA's Hubert H. Humphrey Award and the Tyler Prize for the Stimulation of Research. He has also received the Hall of Distinguished Alumni Lifetime Achievement Award from the University of Kentucky College of Pharmacy, the Weaver Medal from the University of Minnesota College of Pharmacy, and the Leadership in Action Award from the Minnesota Health Action Group. Schondelmeyer earned his BSPharm from the University of Missouri-Kansas City (1974), an ASHP Residency and Doctor of Pharmacy from the University of Kentucky (1977), and master's in public administration (1979) and PhD in pharmacy administration (1984) from The Ohio State University.
For every pharmacist, for all of pharmacy.
SOURCE American Pharmacists Association
WANT YOUR COMPANY'S NEWS FEATURED ON PRNEWSWIRE.COM?
440k+
Newsrooms &
Influencers
9k+
Digital Media
Outlets
270k+
Journalists
Opted In
GET STARTED
03 Jun 2024
Successful first-in-human study shows YCT-529 is safe
SAN DIEGO--(BUSINESS WIRE)-- 2024 BIO International Convention—YourChoice Therapeutics, Inc., pioneering hormone-free family planning products, has completed its first-in-human clinical study for YCT-529, designed to be the first hormone-free birth control pill for men. YourChoice Therapeutics CEO Akash Bakshi will present the results of the phase 1a study at the 2024 BIO International Convention on June 4 at 10:45 PDT.
“We’re one step closer to delivering the world’s first male birth control pill,” said YourChoice Therapeutics chief science officer Nadja Mannowetz. “While the road to FDA approval for any new drug candidate is long, we’re very pleased with the speed, efficiency, and enthusiasm for YCT-529’s first-in-human study. The findings are powerful validation that YCT-529 is safe and well tolerated in men and lays a favorable foundation for further studies.”
Innovation in birth control has been stagnant since the female birth control pill (“the Pill”) debuted 65 years ago. Since then, all new birth control options, except for the copper IUD, have relied on dosing women with hormones to prevent pregnancy. Importantly, there have been no new options for men, reinforcing the view that pregnancy prevention is “a woman’s job.” A birth control pill for men that’s hormone-free is a transformative innovation for a very deserving healthcare segment. In YCT-529’s phase 1a study, researchers studied doses up to 180 mgs, finding that all were safe and well tolerated. The next study will investigate multiple ascending doses (MAD) in a larger participant pool. YCT-529’s preclinical studies showed it was 99% effective and 100% reversible with no side effects.
“The Pill turns 65 next year, marking more than a half-century of hormonal birth control with no new options for men to reduce the hormonal burden on their partners,” said Stewart McCallum, MD FACS, chief medical Officer for YourChoice Therapeutics, Inc. “This lack of modernization would be unacceptable in any area of healthcare and motivates us to advance YCT-529, which is on track to be the first hormone-free male birth control pill. The success of our phase 1a study is an important milestone on the path to delivering innovation in birth control that will benefit men and women alike.”
YCT-529 is a retinoic acid receptor-alpha (RAR-alpha) inhibitor, which prevents sperm production by blocking access to vitamin A in the testes. Researchers discovered this mechanism of action in the 1930s after discovering that depriving mice, rats, and monkeys of vitamin A caused infertility. Since that time, decades of published studies have validated the pathway.
“Women’s narrowing reproductive rights offer potent fuel to the fire driving male contraceptive candidates,” said YCT-529 Developer Gunda Georg, regents professor at the University of Minnesota’s College of Pharmacy and founding director of the Institutes for Therapeutics Discovery and Development. “Numerous published studies and surveys show that the world wants and needs more male contraceptive options. We also can’t deny that women are tired of bearing the burden of hormones. I’m very pleased by the speed and efficiency of YCT-529’s first-in-human study and feel confident that future studies will demonstrate similar success. Society is ready for a male contraceptive, and we applaud the organizations that recognize this and support our efforts to deliver the first hormone-free male birth control pill.”
Quotient Sciences, based in the UK, conducted the phase 1a study, which began in December 2024.
About YCT-529
Researchers have understood for decades that vitamin A is essential for male fertility. YCT-529 is a retinoic acid receptor-alpha (RAR-a) inhibitor that prevents production of sperm cells in the testes as well as their release by blocking RAR-alpha (one of three nuclear receptors that bind retinoic acid, a form of vitamin A). Preclinical studies have shown that YCT-529 is 99% effective at preventing mouse pregnancies and 100% reversible. YourChoice Therapeutics developed YCT-529 in collaboration with Dr. Gunda Georg, a globally recognized medicinal chemist and awardee of one of the largest NIH-funded Contraceptive Centers. The Male Contraceptive Initiative (MCI) has been committed to funding the early research and YCT-529’s phase one clinical trial in men. More information about the trial can be found at clinicaltrials.gov, NCT06094283.
About YourChoice Therapeutics
YourChoice Therapeutics is a clinical-stage biopharmaceutical company developing the first hormone-free birth control pill for men. Based in San Francisco, the company is advancing the only male pill in human studies. Preclinical studies showed YCT-529 performed as effectively or better than the female birth control pill. Future programs will apply the company’s patented therapeutic platform to develop hormone-free family planning products for women. Established in 2018, the company received a $15M Series A investment in 2022. For more information, visit and follow the company on LinkedIn.
Phase 1Phase 2
100 Deals associated with University of Minnesota College of Pharmacy
Login to view more data
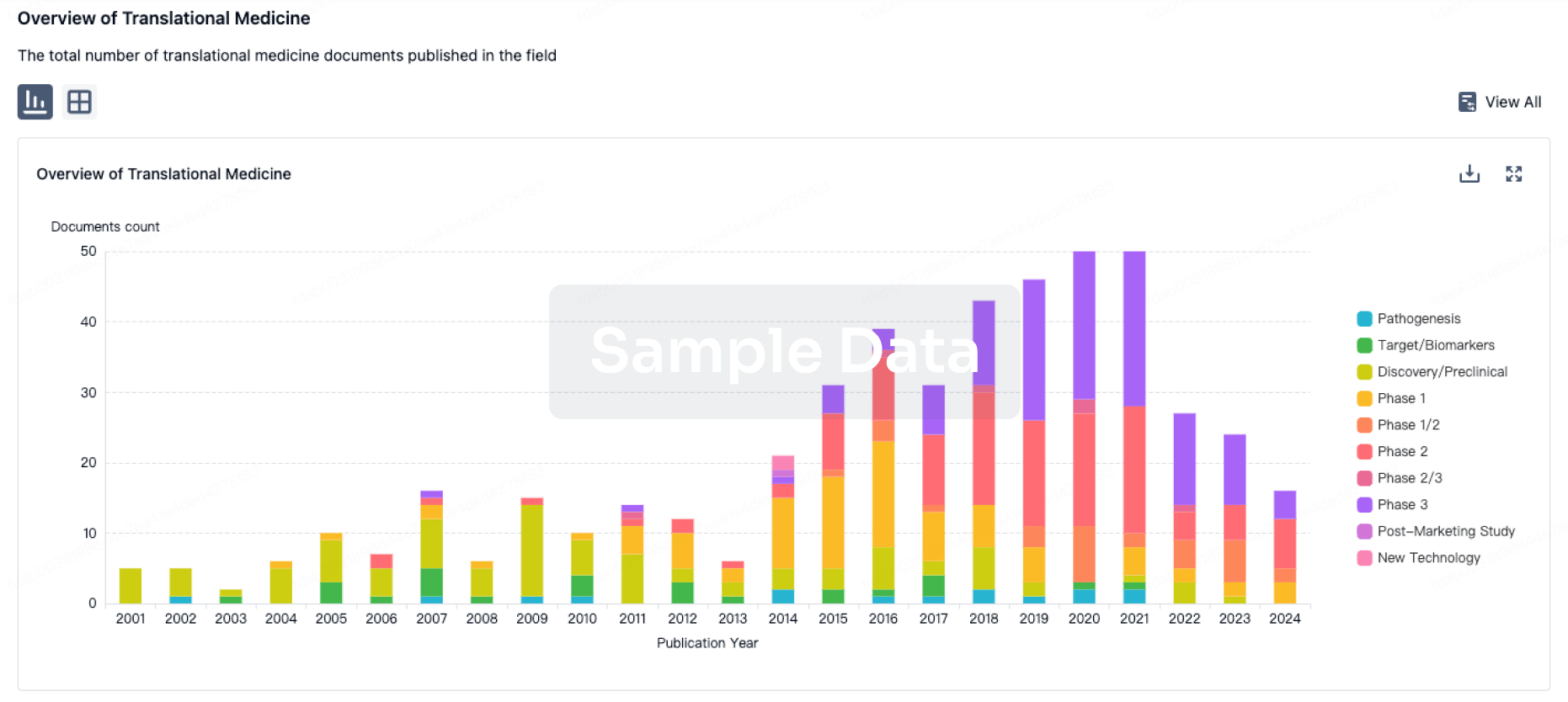
100 Translational Medicine associated with University of Minnesota College of Pharmacy
Login to view more data
Corporation Tree
Boost your research with our corporation tree data.
login
or

Pipeline
Pipeline Snapshot as of 18 May 2025
No data posted
Login to keep update
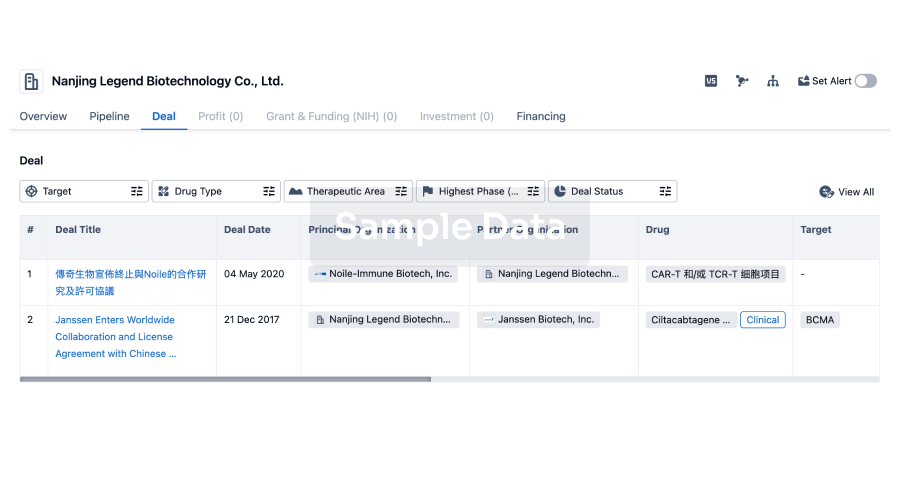
Deal
Boost your decision using our deal data.
login
or
Translational Medicine
Boost your research with our translational medicine data.
login
or
Profit
Explore the financial positions of over 360K organizations with Synapse.
login
or

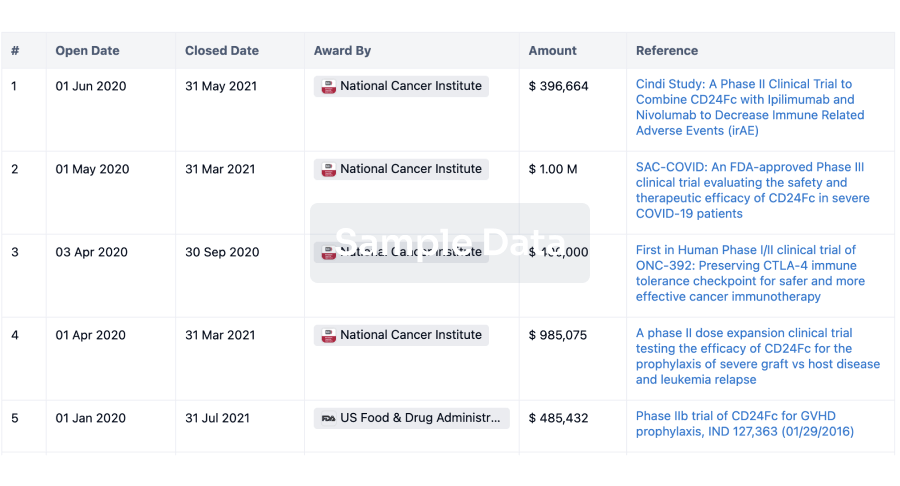
Grant & Funding(NIH)
Access more than 2 million grant and funding information to elevate your research journey.
login
or
Investment
Gain insights on the latest company investments from start-ups to established corporations.
login
or

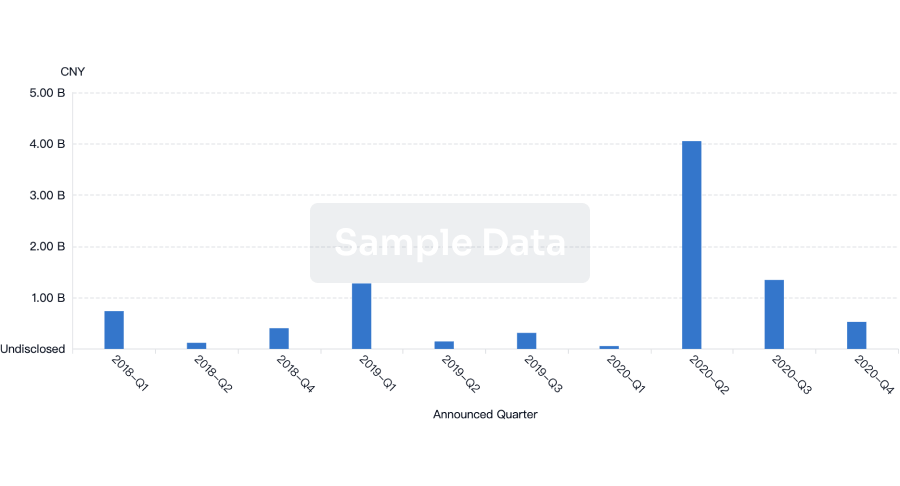
Financing
Unearth financing trends to validate and advance investment opportunities.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free