Request Demo
Last update 08 May 2025

OmniSeq, Inc.
Last update 08 May 2025
Overview
Related
100 Clinical Results associated with OmniSeq, Inc.
Login to view more data
0 Patents (Medical) associated with OmniSeq, Inc.
Login to view more data
83
Literatures (Medical) associated with OmniSeq, Inc.01 Sep 2024·Cancer and Metastasis Reviews
OX40/OX40 ligand and its role in precision immune oncology
Review
Author: DePietro, Paul ; Nishizaki, Daisuke ; Conroy, Jeffery M ; Miyashita, Hirotaka ; Pabla, Sarabjot ; Kato, Shumei ; Nesline, Mary K ; Kurzrock, Razelle ; Lee, Suzanna ; Thapa, Bicky ; Previs, Rebecca A
01 Jun 2024·Journal of Clinical Oncology
Novel HLA-Ilo/HLA-IIhi phenotype and immune evasion in triple-negative breast cancer.
Author: Previs, Rebecca A. ; Gandhi, Shipra ; Hastings, Stephanie B ; Conroy, Jeffrey M ; Ko, Heidi Chwan ; Strickland, Kyle C ; DePietro, Paul ; Pabla, Sarabjot ; Senosain, Maria-Fernanda ; Dash, Durgapras ; Van Roey, Erik ; Caveney, Brian ; Pulivendula, Yamuna ; Parikh, Hardik ; Severson, Eric A ; Nesline, Mary K ; Jensen, Taylor J. ; Gao, Shuang ; Ramkissoon, Shakti H ; Seager, R.J.
01 Jun 2024·Journal of Clinical Oncology
Use of CRTAM expression as a predictive biomarker for immune checkpoint blockade in a pan-cancer cohort.
Author: Aoshima, Ken ; Conroy, Jeffrey M ; DePietro, Paul ; Lee, Suzanna ; Kato, Shumei ; Pabla, Sarabjot ; Miyashita, Hirotaka ; Kurzrock, Razelle ; Nishizaki, Daisuke ; Nesline, Mary K
3
News (Medical) associated with OmniSeq, Inc.09 Nov 2022
SAN DIEGO--(
BUSINESS WIRE
)--
Pleno Inc.,
a multi-omic instrument platform company revolutionizing biological target detection for clinical testing and biomedical research, announced that Mark Gardner has joined its Board of Directors. Gardner joins Chairman, Gregory T. Lucier, Kim Kamdar, Andrew ElBardissi, Vik Barjaj, and Pieter van Rooyen, Pleno’s CEO. In October, Pleno announced a
$40 million Series A
funding round, led by Deerfield Management with participation by Foresite Capital.
Gardner brings more than 30 years of senior management experience to Pleno. He is a proven business leader, with successful endeavors in globally renowned early stage and well-established businesses. He is currently Senior Vice President of Molecular Genomics and Oncology at Quest Diagnostics, where he is responsible for driving growth for Quest’s Advanced Diagnostics offerings by providing genetic sequencing services and cancer diagnostics, working closely with all clinical franchises. Previously, Gardner served as Senior Vice President at Corza Health and as the Chief Executive Officer of OmniSeq. Prior to that, he spent more than 12 years in various executive roles at Thermo Fisher Scientific (previously Life Technologies), including the Vice President and General Manager of the Ion Torrent business unit.
“We are incredibly fortunate to have someone of Mark’s caliber and experience join our Board at Pleno,” said Pieter van Rooyen, Founder and CEO of Pleno. “His deep industry understanding, combined with his ability to translate strategy into exceptional execution, will bring immense value to us as we continue to push the boundaries of what can be done with biological target detection.”
Pleno’s Hypercoding
TM
technology enables a wide array of multi-omic, known-content applications, such as early cancer screening, non-invasive prenatal testing, newborn screening, large-scale infectious disease panels, proteomics, agrigenomics and more, to be democratized and scaled at a rate required to support a global population approaching 8 billion. Developers of these applications can utilize Pleno’s technology to rapidly deploy low-cost, high throughput and multiplexed assays at a scale, which was previously unachievable. RAPTOR
TM
, Pleno’s Hypercoding instrument platform, will be available for early customer access in 2023, with commercial availability in 2024.
“Pleno’s potential to directly address the significant unmet need in the proliferating multi-omics space is truly impressive,” said Mark Gardner, member of Pleno’s Board of Directors. “I look forward to supporting this all-star team in executing on their vision, as well as guiding the future direction and growth of the company.”
Pleno is based in San Diego’s Sorrento Mesa innovation hub proximate to a robust talent pool of experienced scientists, telecommunication engineers, and biotechnology innovators. The company currently employs 28 full-time employees and plans to continue to grow its team rapidly in the coming months.
About Pleno Inc.
Pleno Inc. is a multi-omic instrument platform company democratizing biological target detection for clinical testing and biomedical research. The company’s proprietary Hypercoding™ technology leverages signal processing techniques from the telecommunications industry to deliver targeted biological information at unprecedented scale, precision, and performance. For more information, visit
www.plenoinc.com
.
29 Apr 2021
Test will be made available to physicians and biopharmaceutical companies through Labcorp
OmniSeq receives New York State approval for OmniSeq INSIGHT genomic and immune profiling test. (Credit: Belova59 from Pixabay)
OmniSeq®, an innovator in next generation sequencing in oncology, today announced the New York State Department of Health’s Clinical Laboratory Evaluation Program has approved the OmniSeq INSIGHTSM test. The test detects genomic variants, genomic signatures, and immune gene expression, providing physicians with clinically actionable evidence to inform therapeutic treatment decisions and identify potential clinical trial options for patients with late-stage solid tumor cancers.
The test will be commercially available to U.S.-based clinicians exclusively through Labcorp and globally to biopharmaceutical companies through Labcorp Drug Development. Throughout Canada, the test will be available through Dynacare, a Labcorp company.
“The launch of OmniSeq INSIGHT represents the continued evolution of our commitment to innovation and to the delivery of the most advanced, comprehensive solid tumor profiling assay,” said Margot Schoenborn, Chief Executive Officer, OmniSeq. “It is designed to detect and characterize the genomic and immune features of patients’ cancer tumors to quickly guide more precise, individualized treatment decisions for patients to ensure they receive the best personalized medicine options available.”
OmniSeq INSIGHT is a tissue-based, next generation sequencing test. It has been clinically and analytically validated for all solid tumors, interrogating gene alterations that are targets identified for therapy. Completely unique to the test is the integration of immune expression profiling, which detects genes involved in the anti-cancer immune response and tumor-immune mechanisms including low-expressing genes involved in inflammatory signaling. The combined profiling of molecular and immune genes delivers an unparalleled and powerful new tool to help physicians more effectively select personalized therapies and immunotherapies, as well as match patients to clinical trials based on multi-immune marker analyses.
OmniSeq INSIGHT delivers the distinct advantage of leveraging three technologies to better inform physicians in selecting the most appropriate therapies or clinical trials for their patients. DNA sequencing is used to detect base substitutions, insertions, deletions, copy number alterations, tumor mutational burden and microsatellite instability. RNA sequencing is employed for detection of known and novel gene arrangements in order to maximize detection of fusion events and gene expression profiling; this also provides differentiating insight into critical tumor-immune interactions. Additionally, PD-L1 expression is measured by immunohistochemistry using FDA-approved assays based on the tumor type tested.
OmniSeq INSIGHT can be used in both diagnostic and drug development settings. It is actively integrated into numerous drug development programs and can be configured as an effective discovery tool, screening tool or clinical trial assay and can drive companion diagnostics development and commercialization initiatives. OmniSeq INSIGHT is offered to global biopharmaceutical customers directly and through Labcorp Drug Development, which collectively have an extensive track record in validating assays across key regulatory standards, including CLIA, CLEP, CE-IVD and FDA under an ISO 13485 quality management system for medical devices.
Source: Company Press Release
28 Jan 2021
BUFFALO, N.Y., Jan. 28, 2021 /PRNewswire/ -- OmniSeq®, an innovator in next generation sequencing in oncology, today announced its collaboration with the University of Pittsburgh Medical Center (UPMC) to employ its RNA sequencing (RNA-seq) gene expression pro for selecting immunotherapy combinations for patients in a Phase II clinical trial for patients with Recurrent/Metastatic (R/M) head and neck squamous cell carcinoma (HNSCC). The primary objective is to better select novel immunotherapeutic combinations by taking a more personalized approach to improve response rates and to further develop better predictive biomarkers of efficacy.
Currently, there is a large need for better therapeutics for patients with HNSCC and other solid tumors after failure of response to anti-PD-1 mAb immunotherapy. This Phase II trial will investigate personalized immunotherapy in R/M HNSCC, by evaluating a patient's tumor microenvironment via immune gene expression by RNA-seq to select the agent (Ipilimumab or Relatlimab) to add to Nivolumab in patients with R/M HNSCC patients that have failed prior immunotherapy.
"We are excited for this collaboration and to be able to offer the gene expression pro to R/M HNSCC patients who have failed prior immunotherapy," said Dr. Dan Zandberg, principal investigator and medical oncology co-leader of the Head & Neck Program at UPMC Hillman Cancer Center. "This trial represents an important first step towards taking a personalized approach to each patient to determine the best combination immunotherapy regimen to use."
The primary objective to be determined through the Phase II trial is the probability of response to treatment when combination immunotherapy treatment is selected based on immune gene expression in R/M HNSCC patients who have progressed on prior anti-PD-1 mAb immunotherapy.
"OmniSeq is pleased that our RNA-seq gene expression assay will be leveraged in Dr. Zandberg's Phase II trial for patient stratification," said Jeffrey Conroy, OmniSeq's Chief Scientific Officer. "Our RNA-seq platform allows data-driven matching of HNSCC patients to the appropriate investigational combination therapy based on the immunological tumor landscape."
Patients who meet eligibility criteria will have tumor tissue obtained and analysis will include OmniSeq's immune gene expression to determine which drug (either Relatlimab or Ipilimumab) will be combined with Nivolumab for treatment.
OmniSeq utilizes a comprehensive immune profiling assay that provides for simultaneous measurement of known and novel immune biomarkers (proteins, RNA, DNA) in solid tumor tissue specimens to support correlative studies, drug development and combination immunotherapy clinical trials. OmniSeq's gene expression pro a component of its OmniSeq Advance® assay, a genomic and immune profiling assay, approved for clinical use by New York State Clinical Laboratory Evaluation Program (NYS CLEP). OmniSeq, Inc. is licensed by CLIA, CAP and the NYS CLEP to perform high-complexity molecular diagnostic testing.
More information about this trial (NCT04326257) is available at .
Contact:
Sawyer Lipari
slipari@lambert.com
ImmunotherapyCollaborate
100 Deals associated with OmniSeq, Inc.
Login to view more data
100 Translational Medicine associated with OmniSeq, Inc.
Login to view more data
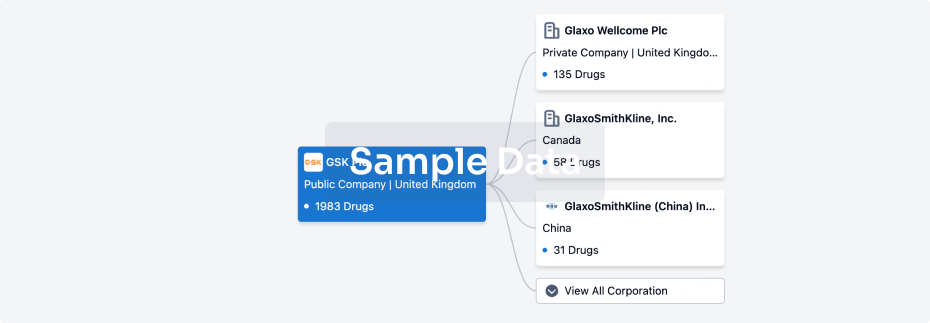
Corporation Tree
Boost your research with our corporation tree data.
login
or
Pipeline
Pipeline Snapshot as of 19 Jul 2025
No data posted
Login to keep update
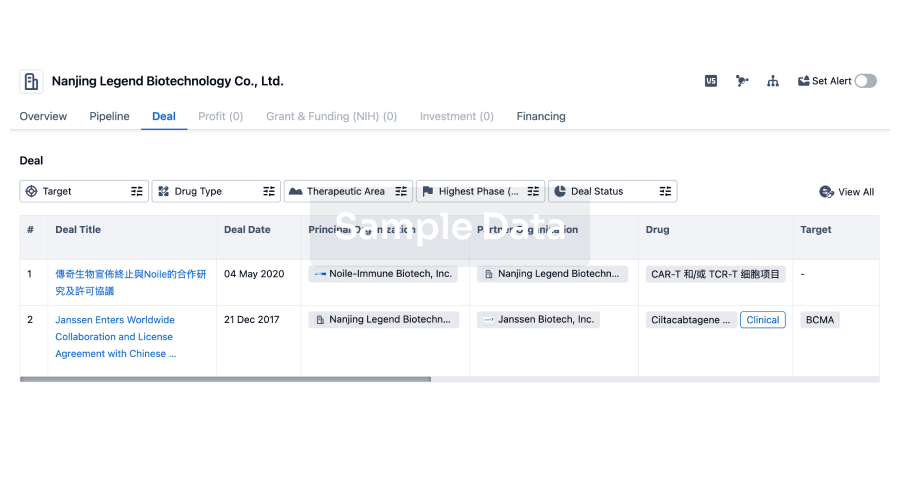
Deal
Boost your decision using our deal data.
login
or
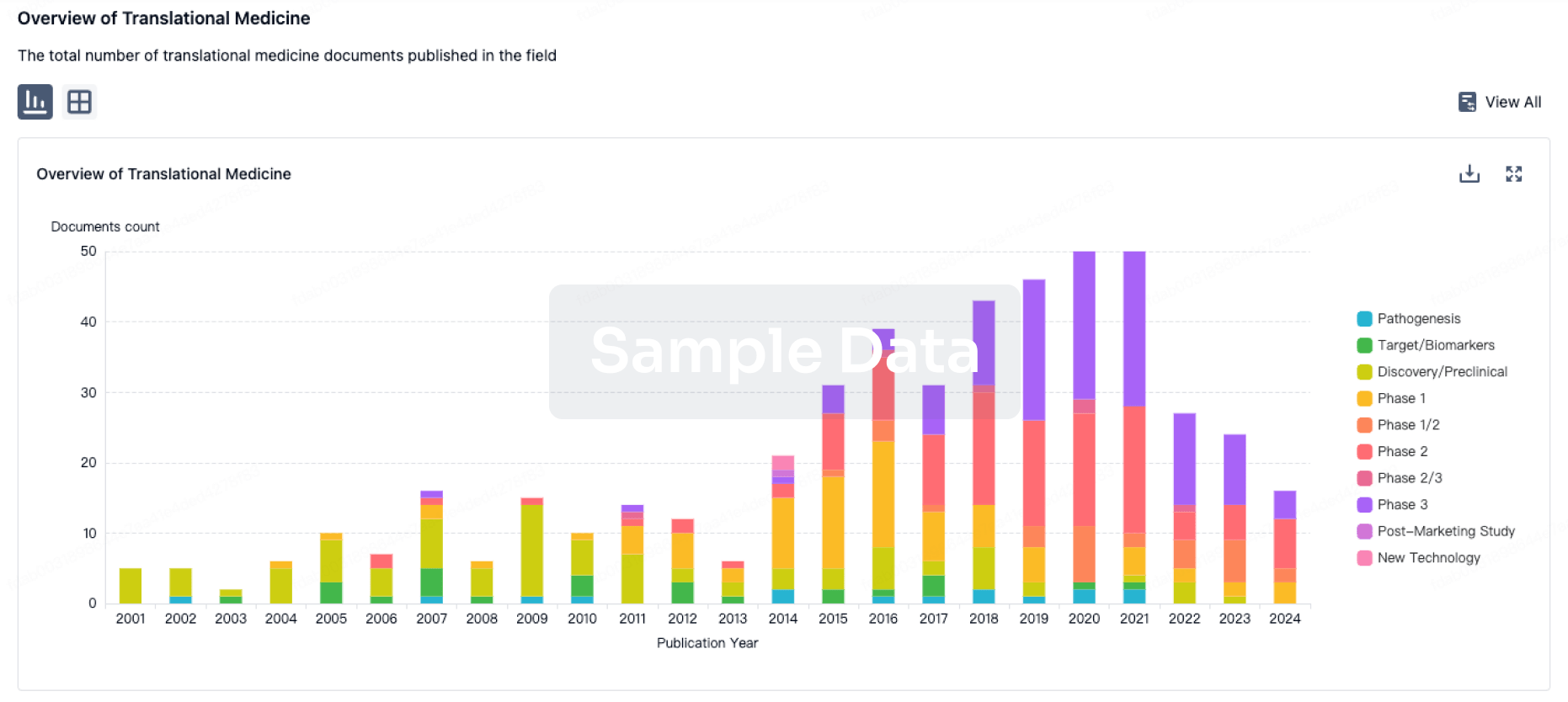
Translational Medicine
Boost your research with our translational medicine data.
login
or
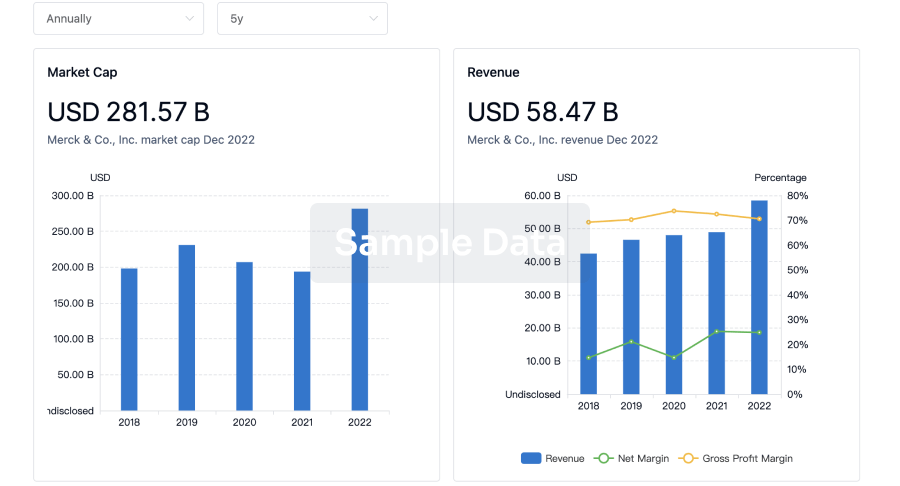
Profit
Explore the financial positions of over 360K organizations with Synapse.
login
or
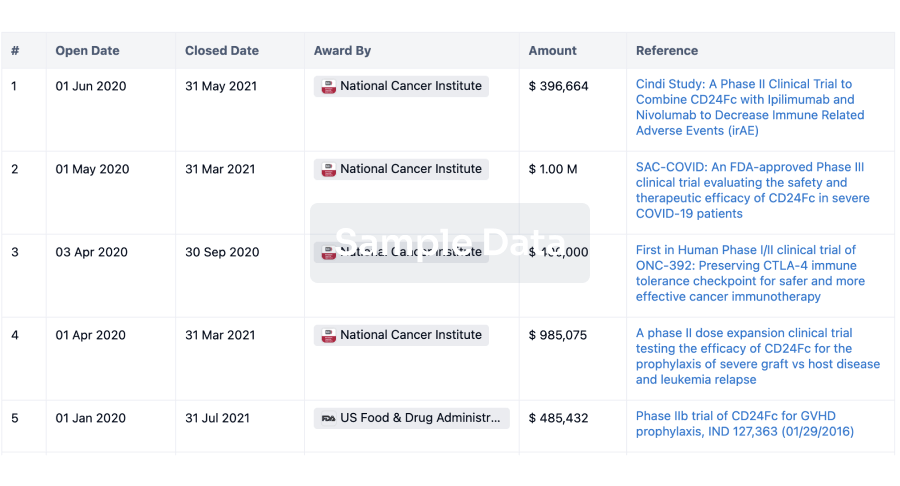
Grant & Funding(NIH)
Access more than 2 million grant and funding information to elevate your research journey.
login
or
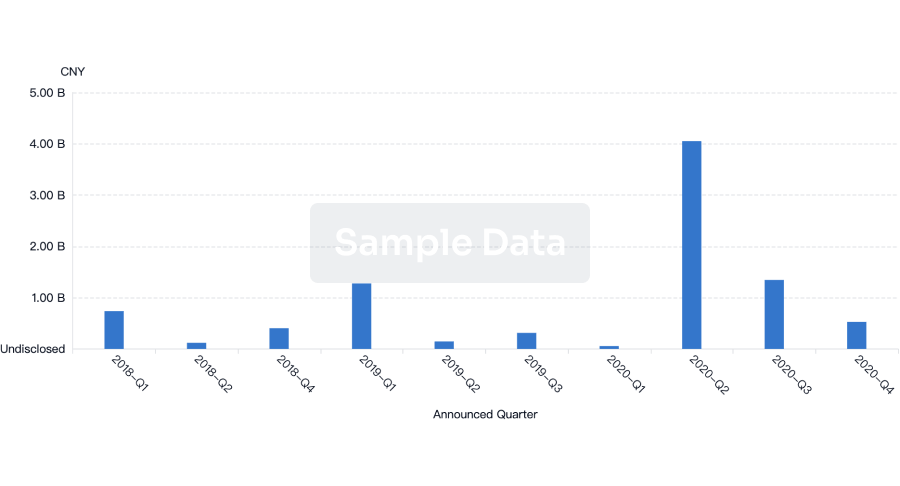
Investment
Gain insights on the latest company investments from start-ups to established corporations.
login
or

Financing
Unearth financing trends to validate and advance investment opportunities.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free