Request Demo
Last update 08 May 2025

Stem Pharm, Inc.
Last update 08 May 2025
Overview
Related
100 Clinical Results associated with Stem Pharm, Inc.
Login to view more data
0 Patents (Medical) associated with Stem Pharm, Inc.
Login to view more data
5
Literatures (Medical) associated with Stem Pharm, Inc.01 Feb 2025·Stroke
Abstract TP211:
In silico
drug repurposing identifies transcriptional mitigators of blood-induced neurotoxicity in an organoid model of intracerebral hemorrhage
Author: Lebakken, Connie ; Richards, William ; Greuel, Kaylie ; Seah, Carina ; Parham, Kailyn ; Schuldt, Braxton ; Kellner, Christopher ; Vicari, James
22 Mar 2024·Cancer Research
Abstract 305: Bioinspired synthetic hydrogel in pancreatic cancer organoid matrix modeling
Author: Lin, Ethan Samuel ; Richards, William ; Lebakken, Connie ; Hossan, Md Shahadat ; Stram, Austin ; McIlwain, Sean ; Kratz, Jeremy D.
01 Feb 2024·Stroke
Abstract 56: Temporal Blood Exposure in Neural Organoids Stimulates Dynamic Astrocyte Reactivity
Author: Lebakken, Connie ; Schuldt, Braxton R ; Seah, Carina ; Vicari, James ; Kellner, Christopher P
2
News (Medical) associated with Stem Pharm, Inc.10 Oct 2023
MADISON, Wis., Oct. 10, 2023 (GLOBE NEWSWIRE) -- Stem Pharm, Inc., a drug discovery platform company leveraging 3D neuro-immune organoids and Verge Genomics, a biotechnology company transforming drug discovery using artificial intelligence (AI) and patient tissue data, announced a collaboration to develop a disease model to validate novel targets identified by Verge for Parkinson’s disease (PD). Parkinson’s disease is a progressive neurodegenerative disorder that affects millions of people worldwide. The complexity and variability of the disease have posed significant challenges in the development of effective therapies. Recognizing the urgent need for innovation, Verge and Stem Pharm have joined forces to leverage cutting-edge human-first technologies and expertise. The collaboration will focus on harnessing the power of neural organoids, which are 3D models of human neural tissue derived from stem cells. Neural organoids provide a unique platform to study the intricacies of the disease and simulate its progression in a laboratory setting. By creating a Parkinson's disease model using neural organoids, the companies aim to gain invaluable insights into the underlying mechanisms of the disease and validate potential drug targets. “We are incredibly excited to partner with Verge to apply our neuro-immune organoid platform to Parkinson’s disease,” said Steven Visuri, CEO of Stem Pharm. “Verge’s all-in-human approach to drug discovery aligns perfectly with our ideology, and by combining our strengths and resources, we aim to establish a state-of-the-art Parkinson’s disease model. This collaboration represents a significant step forward in our collective mission to discover transformative therapies for patients suffering from this debilitating disease.” Stem Pharm’s innovative 3D human neuro-immune organoids feature microglia, the brain’s resident immune cells, making them particularly suited to study diseases associated with neuroinflammation, such as neurodegenerative diseases including Parkinson’s disease and Alzheimer’s disease. These diseases have limited options for therapeutic interventions and are associated with some of the lowest drug approval rates. Stem Pharm is changing the drug discovery paradigm for these diseases by developing physiologically relevant human biology for use in early drug discovery to explore disease pathways, identify and validate novel targets, and discover new therapeutic candidates. About Verge Genomics Verge is focused on developing therapeutics for complex diseases with high unmet need, using human multi-omics from patient disease tissues and machine learning. Verge has created CONVERGE™, a proprietary all-in-human platform, featuring one of the field’s largest and most comprehensive databases of multi-omic patient data. The company is led by experienced computational biologists and drug developers who are successfully advancing clinical and preclinical therapeutic programs in various diseases, including ALS and Parkinson’s disease. For additional information, please follow us on LinkedIn and Twitter. About Stem Pharm Stem Pharm is a neurological drug discovery platform company developing the next-generation of neurologic drugs using a human-first approach. Stem Pharm’s proprietary drug discovery platform is based on human 3D neuro-immune organoids that feature microglia and model neuroinflammation, which play a critical role in many neurological diseases. The company applies this platform to discover and validate disease targets and therapeutics for its internal programs in epilepsy, neurodegeneration, and brain cancer as well as for its biopharma partners’ therapeutic programs. Stem Pharm is based in Madison, WI, a hub for innovative stem cell and biosciences research. For more information, visit stempharm.com and follow us on LinkedIn. Media and Investors:For Verge Genomics:Adam SilversteinScient PRadam@scientpr.com For Stem Pharm:Ryan Gordon, Ph.D.ryan.gordon@stempharm.com
18 Jan 2023
Joining the cohort in Cambridge, MA, Perceiv AI will receive direct funding and mentorship from Merck, Northpond Ventures, and McKesson Ventures to advance its prognostic platform focused on multimodal data in neurodegenerative diseases.
BOSTON, Jan. 17, 2023 /PRNewswire/ - Perceiv AI announced that the company has been selected by Merck (NYSE: MRK) for the inaugural Merck Digital Sciences Studio (MDSS) cohort, along with eight other early-stage biomedical startups from a pool of 152 applicants. The program started in November to fuel innovative digital technologies for drug discovery and development.
"Being selected for the Merck MDSS program is a major accomplishment for Perceiv AI and a testament to the hard work and dedication of our team. This partnership is a huge step forward for us and we are grateful for this opportunity," said CEO and co-founder Dr. Christian Dansereau. "We are excited to work alongside such a renowned and respected company in the healthcare and life sciences industry and to use our cutting-edge AI technology to make a real impact in the field to advance pharma R&D innovation for clinical development, patient identification, clinical trial optimization, and trial de-risking."
MDSS is a collaboration between Merck and the New Jersey Innovation Institute, with investments from the Merck Global Health Innovation Fund, Northpond Ventures, and McKesson Ventures. The accelerator provides direct investment from Merck, access to powerful Azure Cloud computing, and technology support provided by Microsoft for Startups. Additionally, participating companies are provided opportunities to collaborate with discovery and clinical scientists at Merck for pilots, where appropriate.
Perceiv AI intends to expand upon its proprietary multimodal prognostic platform ForesightTM through the program. The ForesightTM platform, which integrates longitudinal clinical data with imaging and genetics to forecast disease progression, supports the development of prognostic biomarkers for neurological diseases, including Alzheimer's disease, for clinical trials and clinical use.
Perceiv AI joins Andson Biotech, Deep Forest Sciences, Gesund.ai, Magna Labs, IndyGeneUS AI, SciMar ONE, Stem Pharm, and Pepper Bio in the 10-month accelerator program. The program will begin with the company's exploration of where its technology can augment Merck's existing focus areas with the goal of transitioning into a pilot project with Merck.
This announcement comes on the heels of Perceiv AI's closing of its financial round at the end of last year. Along with strategic partners and investors like the one in this program, Perceiv AI will be able to further develop its ForesightTM platform.
To learn more about Perceiv AI, please visit .
About Perceiv AI
Perceiv AI is an AI-driven precision medicine company developing a powerful multimodal prognostic platform to forecast disease progression in age-related diseases like Alzheimer's. By providing a window into individual patients' disease progression, Perceiv AI aims to accelerate and de-risk the development of new therapies while enabling timelier diagnoses.
About Merck
Merck, also known as MSD outside of the United States and Canada, strives to be the premier research-intensive biopharmaceutical company through a diverse and inclusive global workforce. For over 130 years, Merck has been using the power of leading-edge science to deliver innovative health solutions to save and improve the health and wellness of people and animals worldwide with important medicines and vaccines.
About New Jersey Innovation Institute
New Jersey Innovation Institute (NJII), a 501c3 subsidiary of NJIT, combines the resources of the university, strong industry and government relationships, and proven methods to drive innovation and deliver transformative products and services that make a direct impact on the economy and the health and welfare of its participants. To achieve this, NJII is organized into four divisions that help turn ideas into workable solutions: healthcare, entrepreneurship, defense and homeland security, and professional and corporate education. More at njii.com.
About Northpond Ventures
Northpond Ventures is a multi-billion-dollar science-driven venture capital firm based in Cambridge, MA; San Francisco, CA; and Bethesda, MD. Northpond has consistently been named one of the most active lead life science investors by both Crunchbase and Silicon Valley Bank. It is deeply engaged in the academic ecosystem, having founded The Laboratory for Bioengineering Research and Innovation at Harvard's Wyss Institute; launched the MIT-Northpond Program - Advancing Life Science & Engineering Innovation; and sponsored a prize for women entrepreneurs at MIT. It has led or co-led over 60 financings over the past several years and sits on the board of the vast majority of these businesses. Learn more at npv.vc.
SOURCE Perceiv AI
100 Deals associated with Stem Pharm, Inc.
Login to view more data
100 Translational Medicine associated with Stem Pharm, Inc.
Login to view more data
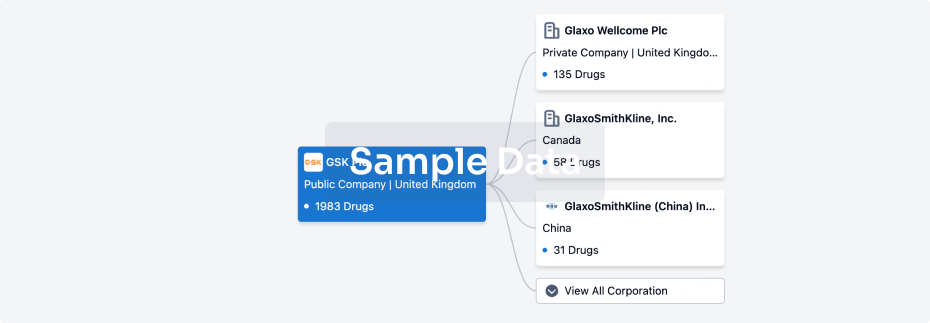
Corporation Tree
Boost your research with our corporation tree data.
login
or
Pipeline
Pipeline Snapshot as of 08 Jun 2025
No data posted
Login to keep update
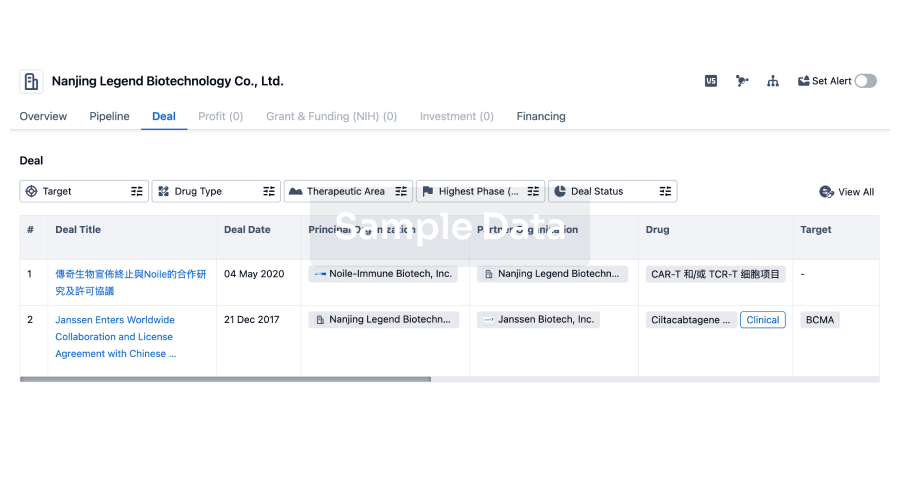
Deal
Boost your decision using our deal data.
login
or
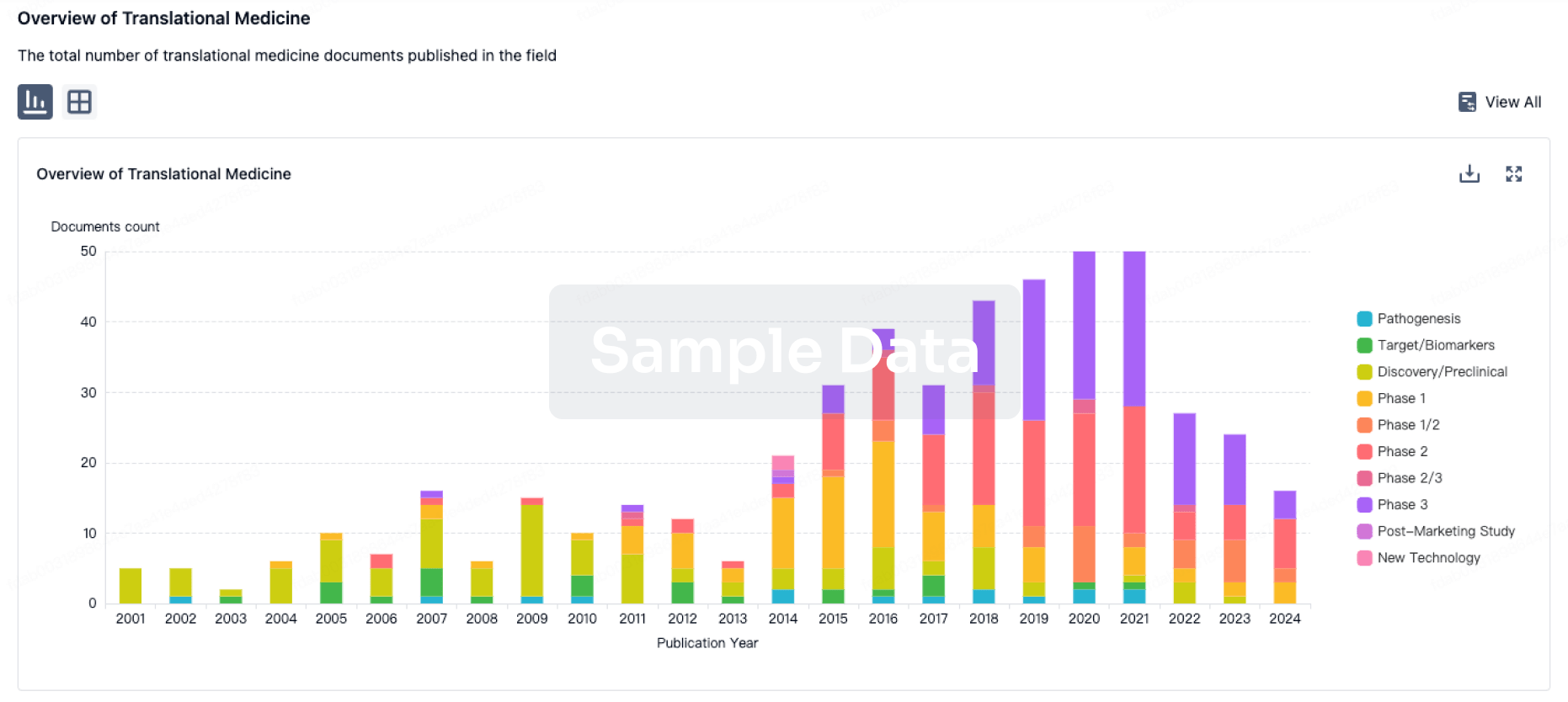
Translational Medicine
Boost your research with our translational medicine data.
login
or
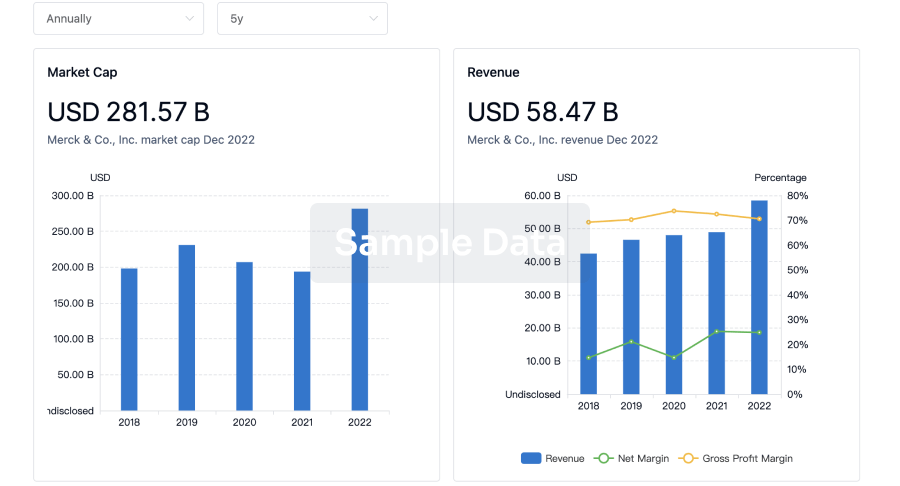
Profit
Explore the financial positions of over 360K organizations with Synapse.
login
or
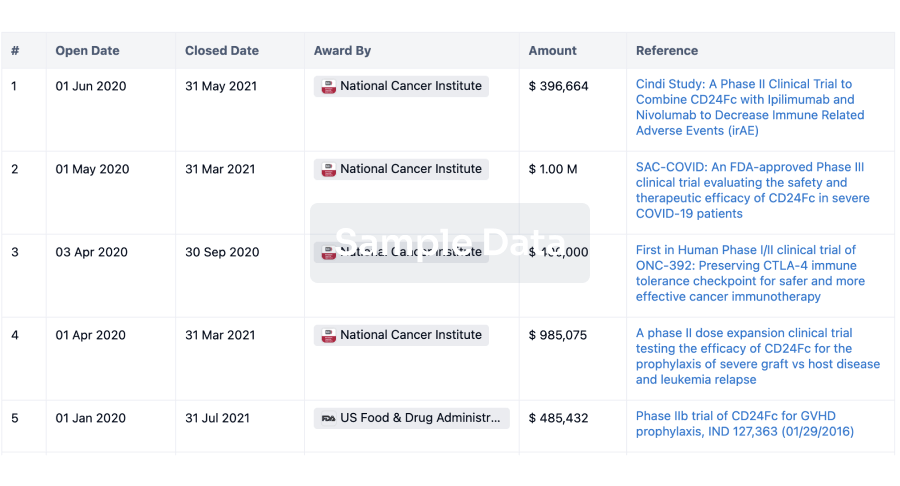
Grant & Funding(NIH)
Access more than 2 million grant and funding information to elevate your research journey.
login
or
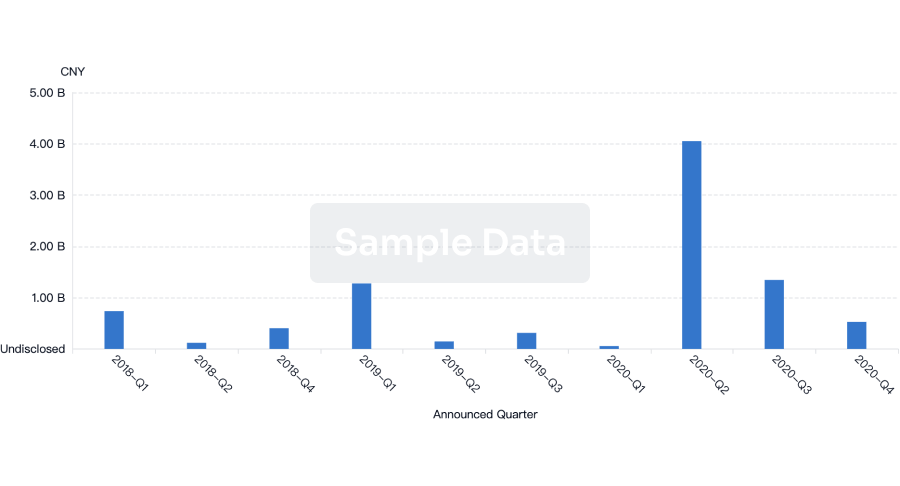
Investment
Gain insights on the latest company investments from start-ups to established corporations.
login
or

Financing
Unearth financing trends to validate and advance investment opportunities.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free