Progress in the Development of Drugs Targeting the PTH1R
In December of 2023, Ascendis Pharma announced that the U.S. FDA has accepted the company's resubmitted New Drug Application (NDA) for palopegteriparatide (TransCon PTH) for the treatment of adult patients with hypoparathyroidism. The resubmitted application constitutes a complete response to the second round of queries, and the Prescription Drug User Fee Act (PDUFA) target date is set for May 14, 2024.
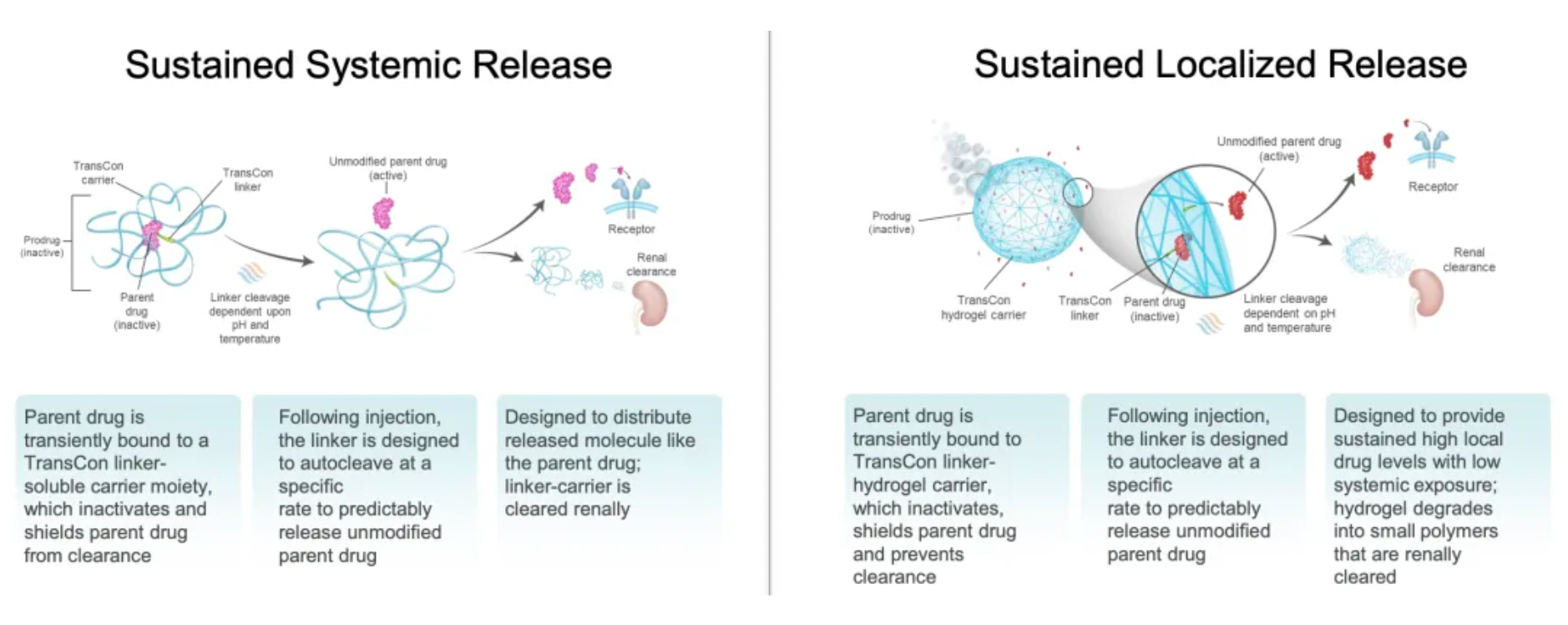
TransCon PTH, developed by Ascendis Pharma, is an investigational prodrug of PTH hormone undergoing research and development. It is a mPEGylated modification of the parathyroid hormone (PTH 1-34) designed for once-daily injection that provides a sustained release of active PTH and is currently in development for the treatment of hypoparathyroidism in adults.
Therapeutic Drugs Targeting PTH1R
The parathyroid hormone 1 receptor (PTH1R) is a member of the Class B G protein-coupled receptor family. This receptor can be activated by two different endogenous peptide agonists, parathyroid hormone (PTH) and parathyroid hormone-related protein (PTHrP), and activates Gs, Gq, and β-arrestin pathways, thereby regulating various signaling pathways and exerting different biological effects.
In November 2023, Apotex announced that the U.S. FDA approved the company's Teriparatide injection for the treatment of osteoporosis. The Teriparatide injection is supplied in a pre-filled pen form for single patient use, containing 250 mcg/mL, with a dosage of 20 mcg per administration.
In November of 2023, the U.S. FDA approved the marketing of Teva Pharmaceuticals' Teriparatide injection, which is also used for the treatment of osteoporosis.
Teriparatide is a recombinant peptide and a synthetic form of the natural human parathyroid hormone. This medication can help the body to form new bone, increase bone mineral density, and enhance bone strength.
Abaloparatide is an N-terminal analog of parathyroid hormone-related peptide (PTHrP) originally researched and developed by Ipsen SA. It is an agonist of the parathyroid hormone 1 receptor (PTH1R), as well as a synthetic 34-amino acid peptide sharing 41% homology with human parathyroid hormone 1-34 and human PTHrP 1-34. Following its approval in the United States in 2017, it has been approved in countries and regions such as Japan and the European Union for the treatment of osteoporosis and postmenopausal osteoporosis.
Currently, there are two PTH1R-targeting candidate drugs for the clinical treatment of hypoparathyroidism in Phase 1 clinical trials: MBX-2109, a PTH1R agonist from MBX Life Sciences, and Chugai Pharmaceutical's PTH1R agonist PCO-371.
In 2016, Chugai Pharmaceutical published an article in the journal Nature Communications on the development of PCO-371, an orally active small molecule PTHR1 agonist for the treatment of hypoparathyroidism. PCO-371 is a novel orally active small molecule and serves as a full agonist of PTHR1. Oral administration of PCO-371 in osteoporotic rats significantly increased bone turnover rates, yet there was a limited increase in bone mass. In hypocalcemic rats, PCO-371 restored serum calcium levels without increasing urinary calcium, and its effects were stronger and more durable than injectable PTH. These results suggest that PCO-371 could offer a new therapeutic option for PTH-related disorders, including hypoparathyroidism.
In July of 2023, GPCR drug discovery startup Septerna announced that the company had secured $150 million in Series B funding to advance the development of a novel pipeline of GPCR-targeted drugs. According to the news release, this round of financing will be used to support the development and clinical mechanism validation of leading programs targeting PTH1R.
About Osteoporosis
Osteoporosis is a skeletal disorder primarily caused by a reduction in bone density and the destruction of bone microarchitecture, leading to bones becoming fragile and prone to fractures. The main symptoms of osteoporosis include susceptibility to fractures, decreased height, back pain, and loss of weight. The goal of osteoporosis treatment is to prevent fractures. At present, clinical targets developed for the treatment of osteoporosis mainly include PTH1R, RANKL, ER, ERα, CALCR, and others.
Bisphosphonates are the most widely used anti-bone resorption drugs, capable of reducing bone turnover markers to low premenopausal concentrations and decreasing fracture rates (vertebral fracture rates by 50%-70%, non-vertebral fracture rates by 20%-30%, and hip fracture rates by approximately 40%). Bisphosphonates can tightly bind with bone mineral and their effects may be eliminated over several months to years.
Denosumab is a monoclonal antibody targeting RANKL that can effectively inhibit the development and activity of osteoclasts. Denosumab is administered subcutaneously every six months. The anti-fracture efficacy of denosumab is similar to that of bisphosphonates, but after the last injection at 7 months, the anti-resorption effect significantly reduces, which may lead to a rebound in vertebral fractures.
Romosozumab is a monoclonal antibody against sclerostin that can stimulate bone formation and inhibit bone resorption. Romosozumab is administered subcutaneously once a month, with a treatment course of 1 year. Head-to-head studies indicate that, compared with anti-resorption drugs, anabolic agents have stronger anti-fracture efficacy, and also a greater increase in bone density. The effects of anabolic agents are transient, thus necessitating a transition to anti-resorption drugs. The optimal cycling strategy involving anabolic agents, anti-resorption drugs, and periods off medication remain to be determined.




