Request Demo
Last update 29 Aug 2025

Pomorski Uniwersytet Medyczny W Szczecinie
Last update 29 Aug 2025
Overview
Related
55
Clinical Trials associated with Pomorski Uniwersytet Medyczny W SzczecinieNCT06614790
Patient Outcomes and Safety of Niraparib as Maintenance Treatment in Patients With Newly Diagnosed Advanced Platinum- Sensitive, Ovarian Cancer. The First Real-World Evidence Study From Poland.
The study is observational, not interventional. The study will include patients with advanced ovarian cancer who have been treated in Poland based on a previous early access program, and who are currently being treated under the B.50 drug program, funded by the National Health Fund.
Only patients currently being treated in the B.50 program at 10 selected centers listed on this site may be included in the study.
Of course, any patient in Poland eligible for maintenance treatment with niraparib can receive the drug, regardless of participation in this RWE study.The treatment involves administering niraparib as maintenance therapy for 3 years after the completion of chemotherapy, provided that the patient has responded to systemic treatment (NED, CR, PR).
Only patients currently being treated in the B.50 program at 10 selected centers listed on this site may be included in the study.
Of course, any patient in Poland eligible for maintenance treatment with niraparib can receive the drug, regardless of participation in this RWE study.The treatment involves administering niraparib as maintenance therapy for 3 years after the completion of chemotherapy, provided that the patient has responded to systemic treatment (NED, CR, PR).
Start Date02 Sep 2024 |
Sponsor / Collaborator |
NCT06223685
Randomized, Double-blind, Placebo-Controlled Study on Efficacy of a Dietary Intervention With Probiotic Bacterial Strains as an Adjunct to Treatment of Small Intestinal Bacterial Overgrowth With Rifaximin
The goal of this clinical trial is to test the effectiveness of probiotic bacterial supplements as an additional therapeutic modality in patients with small intestine bacterial overgrowth who receive oral antibiotic treatment (rifaximin)
The main questions it aims to answer are:
1 To evaluate the effectiveness of a dietary intervention using pro-biotic bacterial strains as an adjunct to treatment of SIBO with rifaximin.
2. Evaluation of ultrasonographic imaging of mesenteric lymph nodes in patients with SIBO.
3. Evaluation of the effect of rifaximin treatment and dietary intervention on non-alcoholic fatty liver disease activity parameters in patients with coexisting NAFLD and SIBO.
According to the study schedule, a total of 3 visits will be made within 3 months. Visit 1, after 6 weeks Visit 2 and after another 6 weeks, Visit 3. Patients will also be invited to a follow-up Visit 4, three months after completing participation in the study.
All study participants will receive treatment recommendations for SIBO in accordance with standard practice - a 14-day antibiotic treatment with Rifaximin.
In addition, a randomly selected half of the study participants will receive probiotic therapy and half a placebo.
* An ultrasound examination of the mesenteric root lymph nodes will be performed at each visit,
* followed by a lier steatosis/fibrosis assessment using SWE elastography or FibroScan.
* Blood sampling is required on each visit. All study participants will receive detailed guidelines during dietary consultations at each visit for the use of a low FODMAP diet.
* Each participant will receive a paper diary on how to assess the severity of bloating and evaluate bowel movements, which must be filled out daily.
* In addition, at the visits the patient will be asked to fill out an additional questionnaire on other gastrointestinal complaints and mental health.
The main questions it aims to answer are:
1 To evaluate the effectiveness of a dietary intervention using pro-biotic bacterial strains as an adjunct to treatment of SIBO with rifaximin.
2. Evaluation of ultrasonographic imaging of mesenteric lymph nodes in patients with SIBO.
3. Evaluation of the effect of rifaximin treatment and dietary intervention on non-alcoholic fatty liver disease activity parameters in patients with coexisting NAFLD and SIBO.
According to the study schedule, a total of 3 visits will be made within 3 months. Visit 1, after 6 weeks Visit 2 and after another 6 weeks, Visit 3. Patients will also be invited to a follow-up Visit 4, three months after completing participation in the study.
All study participants will receive treatment recommendations for SIBO in accordance with standard practice - a 14-day antibiotic treatment with Rifaximin.
In addition, a randomly selected half of the study participants will receive probiotic therapy and half a placebo.
* An ultrasound examination of the mesenteric root lymph nodes will be performed at each visit,
* followed by a lier steatosis/fibrosis assessment using SWE elastography or FibroScan.
* Blood sampling is required on each visit. All study participants will receive detailed guidelines during dietary consultations at each visit for the use of a low FODMAP diet.
* Each participant will receive a paper diary on how to assess the severity of bloating and evaluate bowel movements, which must be filled out daily.
* In addition, at the visits the patient will be asked to fill out an additional questionnaire on other gastrointestinal complaints and mental health.
Start Date01 Apr 2023 |
Sponsor / Collaborator |
NCT05570097
Cryoanalgesia in Combination With the Novel Prehabilitation Program Back on Feet Are the Essential Parts of Enhanced Recovery Protocol in the Minimal Invasive Modyfied Nuss Procedure of Children With Funnel Chest Deformation.
This Study study compared standard therapy (multimodal and regional analgesia) versus a novel approach (Cryoanalgesia combined with bilateral erector spine plane block and multimodal analgesia) in subjects undergoing minimal invasive modyfied Nuss procedure (thoracoscopy).
Start Date28 Sep 2022 |
Sponsor / Collaborator |
100 Clinical Results associated with Pomorski Uniwersytet Medyczny W Szczecinie
Login to view more data
0 Patents (Medical) associated with Pomorski Uniwersytet Medyczny W Szczecinie
Login to view more data
4,784
Literatures (Medical) associated with Pomorski Uniwersytet Medyczny W Szczecinie01 Jan 2026·CLINICA CHIMICA ACTA
The role of lipidomics in psoriasis
Review
Author: Skórka, Patryk ; Boboryko, Dominika ; Pawlik, Andrzej ; Bratborska, Aleksandra Wiktoria
BACKGROUND:
Psoriasis is a chronic autoinflammatory skin disease marked by keratinocyte hyperproliferation and systemic inflammation. This condition significantly increases the risk of cardiometabolic complications such as atherosclerosis, thromboembolic events, and worsened cardiovascular outcomes. In recent years, metabolomics-particularly lipidomics-has emerged as a powerful approach for elucidating the metabolic dysregulation associated with psoriasis. Lipidomic techniques, including Ultra Performance Liquid Chromatography coupled with Tandem Mass Spectrometry (UPLC-MS/MS), Gas Chromatography-Mass Spectrometry (GC-MS), and UPLC-Quadrupole Time-of-Flight MS (UPLC-QTOF-MS), have enabled the detection and quantification of disease-relevant lipid species. Despite advancements, the inherent structural complexity and diversity of lipid molecules present substantial analytical challenges, particularly in method standardization and cross-study comparison. Nonetheless, specific lipid classes play a central role in the pathogenesis of psoriasis. Additionally, fatty acids and their bioactive metabolites modulate cutaneous inflammation and skin barrier function. A comprehensive understanding of lipid metabolic alterations in psoriasis is critical for identifying novel diagnostic biomarkers and developing targeted therapies aimed at restoring lipid homeostasis and improving clinical outcomes.
AIMS:
The aim of the review is to identify and characterize lipid profile alterations in psoriasis patients and to evaluate the potential of pro-inflammatory lipids as biomarkers of disease activity and treatment response using advanced lipidomic techniques.
01 Oct 2025·SCHIZOPHRENIA RESEARCH
Social disconnection and psychotic-like experiences in daily life: Unravelling the mediating role of threat anticipation
Article
Author: Gawęda, Łukasz ; Misiak, Błażej ; Piotrowski, Patryk ; Grąźlewski, Tomasz ; Bogudzińska, Bogna ; Samochowiec, Agnieszka ; Gelner, Hanna ; Samochowiec, Jerzy
Social disconnection, manifesting as social isolation and/or loneliness, might be associated with psychotic-like experiences (PLEs). There is evidence that lonely individuals tend to focus on social threats instead of searching for opportunities to reconnect with others. Following these considerations, aims of the present study were as follows: (1) to assess momentary patterns of social disconnection in people with PLEs and (2) to test the hypothesis that threat anticipation bias mediates the association between momentary social disconnection and PLEs. The study included 99 individuals with PLEs and 102 controls (individuals without PLEs) who were enrolled from the general population. Participants provided the experience sampling method (ESM) data over 7 consecutive days (6 assessments per day). The ESM questionnaires covered the level of momentary PLEs, threat anticipation, negative affect, solitude, and loneliness. After adjustment for age, sex, and negative affect, individuals with PLEs reported significantly higher rates of momentary loneliness, but not solitude. Also, the inertia (the level of autocorrelation between consecutive assessments) of loneliness, but not solitude, was significantly higher among individuals with PLEs. Threat anticipation mediated the association between momentary loneliness and PLEs across within-person (partial mediation) and between-person (full mediation) models. However, this effect was not significant for the association of momentary solitude with PLEs. The findings indicate that individuals with PLEs experience higher levels of loneliness that tend to persist over time. Threat anticipation plays an important role in shaping the association between loneliness and PLEs.
01 Oct 2025·Lancet Regional Health-Europe
Diagnostic accuracy and predictive value of the QuantiFERON-TB gold plus assay for tuberculosis in immunocompromised individuals: a prospective TBnet study
Article
Author: Dominguez, José ; Nitschke, Martin ; Oral, Haluk Barbaros ; Martinez, Leonardo ; Goletti, Delia ; Avsar, Korkut ; Altet-Gomez, Neus ; Bakken Kran, Anne-Marte ; Crudu, Valeriu ; Matteelli, Alberto ; Palacios-Gutiérrez, Juan José ; Pedersen, Ole Skouvig ; Rupp, Jan ; Dyrhol-Riise, Anne Ma ; Kalsdorf, Barbara ; Hoffmann, Harald ; Lange, Berit ; Bothamley, Graham ; Nordholm Breschel, Anne Christine ; de Souza Galvao, Malu ; Milkiewicz, Piotr ; Chesov, Dumitru ; Toader, Corina ; Villar-Hernandez, Raquel ; van Leth, Frank ; Petruccioli, Elisa ; Duarte, Raquel ; Ibraim, Elmira ; Neyer, David ; Arias-Guillén, Miguel ; Ciobanu, Nelly ; Lange, Christoph ; Ravn, Pernille ; Cirillo, Daniela Maria ; Lipman, Marc ; Kunst, Heinke ; Wagner, Dirk ; Sester, Martina ; Raszeja-Wyszomirska, Joanna ; Dilektasli, Asli Görek ; Spohn, Hanna-Elisa ; Andersen, Åse Bengaard ; Brown, James ; Krawczyk, Marcin
Background:
In low tuberculosis (TB)-endemic countries, tuberculosis preventive therapy (TPT) is recommended for immunocompromised individuals with a positive immunodiagnostic test. This study aimed to assess the performance of the QuantiFERON-TB Gold Plus (QFT+) assay and predictive power for future tuberculosis in immunocompromised individuals.
Methods:
In this prospective observational study, immunocompromised adults ≥18 years of age including people living with HIV (PLHIV), chronic renal failure, rheumatoid arthritis, solid-organ transplantation or stem-cell transplantation, and immunocompetent adults with and without TB-disease were recruited at 21 sites in 11 European countries and tested with the QFT+ assay. Individuals without TB-disease were followed up for the development of tuberculosis. TB incidence rates (IR) were calculated, stratified by QFT+ results and acceptance of TPT. This study is registered with Clinicaltrials.gov, NCT02639936.
Findings:
A total of 2663 individuals (1115 female, 1548 male) were enrolled from 03/11/2015 to 29/03/2019. Persons without tuberculosis were followed up for at least two years. Among 1758 immunocompromised individuals without active tuberculosis, 13.6% had positive QFT+ results. Sensitivity and specificity for TB-disease were 70.0% (52.1-83.3%) and 91.4% (89.6-92.9%), respectively, in immunocompromised, and 81.4% (76.6-85.3%) and 96.0% (92.5-97.9%), respectively, in immunocompetent individuals. During 2457 cumulative years of follow-up among 932 individuals with chronic renal failure, rheumatoid arthritis, solid-organ transplantation or stem-cell transplantation, including 83 persons with a positive QFT+ test without TPT, no-one developed active tuberculosis. In contrast, among 642 PLHIV without TPT, one with an indeterminate QFT+ and 3/30 individuals with a positive QFT+ developed active tuberculosis; all had detectable HIV-replication and low CD4 T-cell counts (incidence 4.1 (95% CI (1.3-12.4) per 100 person-years). No individuals receiving TPT developed active tuberculosis during 269 years of follow-up.
Interpretation:
In immunocompromised individuals in low TB-endemic countries, the 2-year-risk for active tuberculosis was highest among PLHIV with detectable HIV-replication and low CD4-counts. In this study, the QFT+ assay did not strongly predict progression to active tuberculosis, which emphasises the need to incorporate additional risk factors.
Funding:
None.
100 Deals associated with Pomorski Uniwersytet Medyczny W Szczecinie
Login to view more data
100 Translational Medicine associated with Pomorski Uniwersytet Medyczny W Szczecinie
Login to view more data
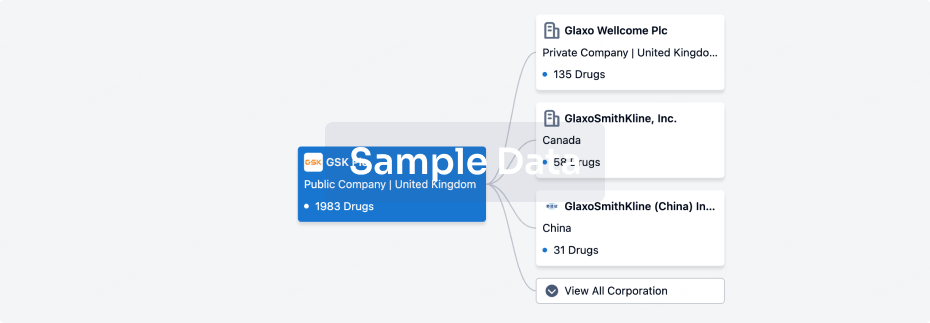
Corporation Tree
Boost your research with our corporation tree data.
login
or
Pipeline
Pipeline Snapshot as of 05 Sep 2025
No data posted
Login to keep update
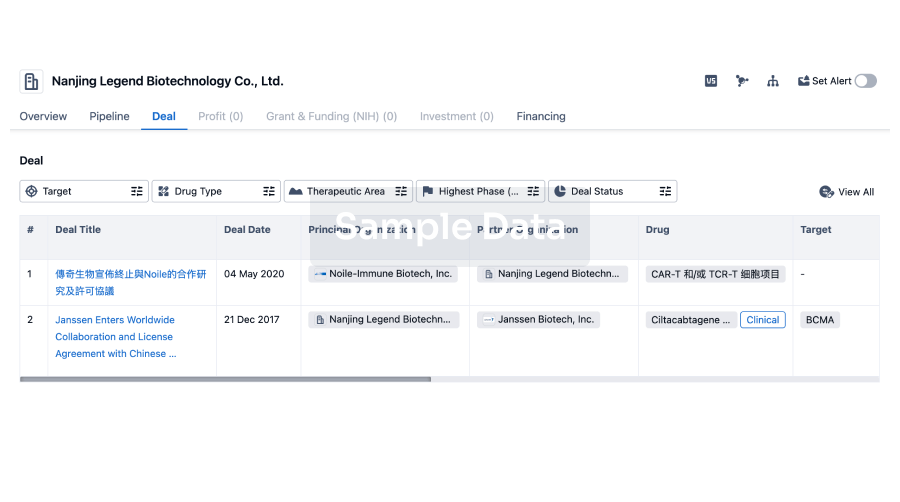
Deal
Boost your decision using our deal data.
login
or
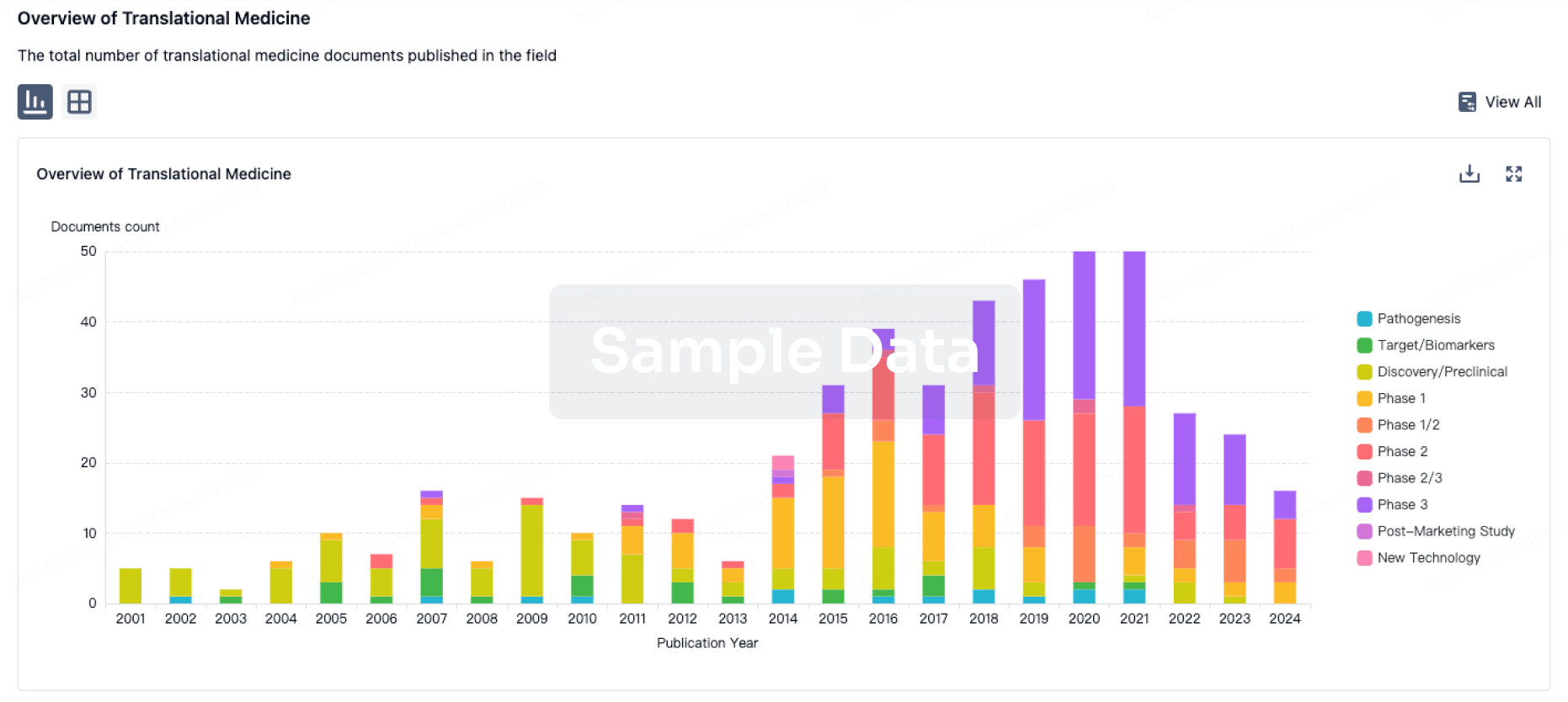
Translational Medicine
Boost your research with our translational medicine data.
login
or
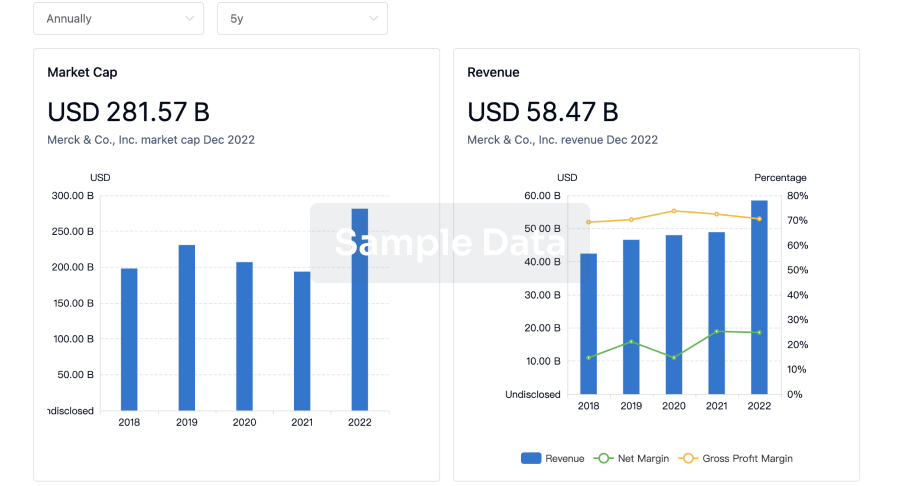
Profit
Explore the financial positions of over 360K organizations with Synapse.
login
or
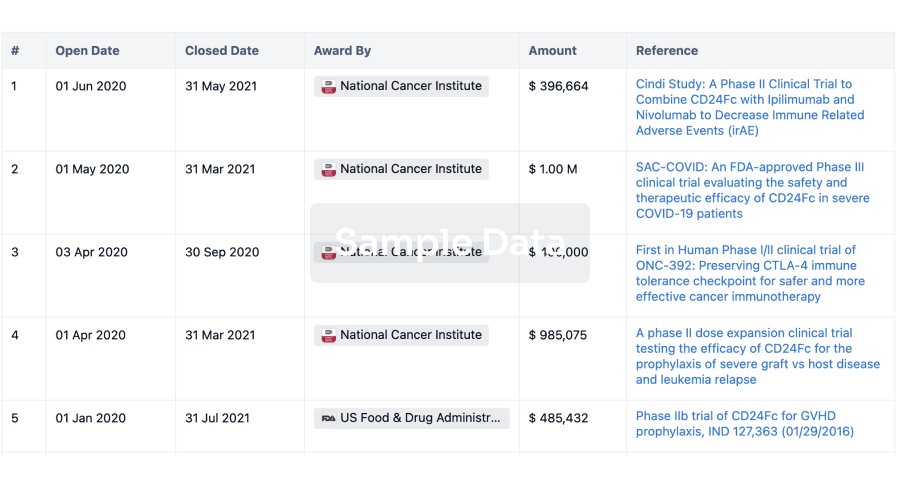
Grant & Funding(NIH)
Access more than 2 million grant and funding information to elevate your research journey.
login
or
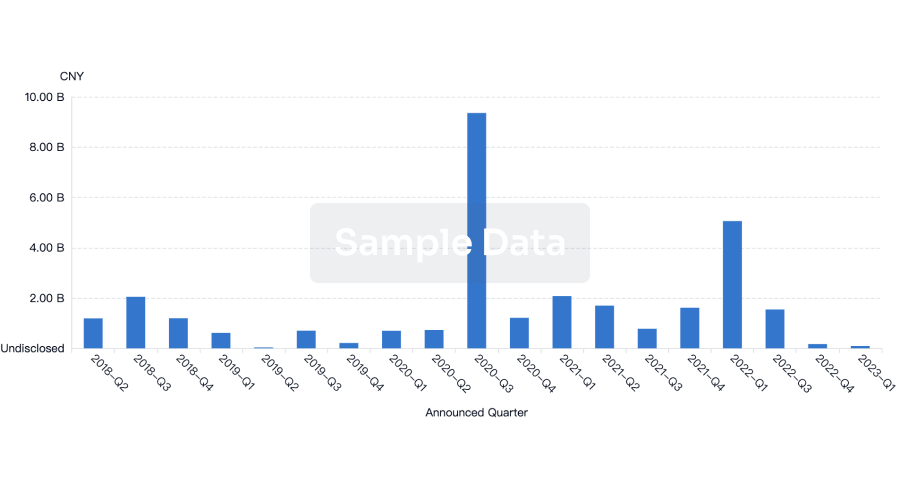
Investment
Gain insights on the latest company investments from start-ups to established corporations.
login
or
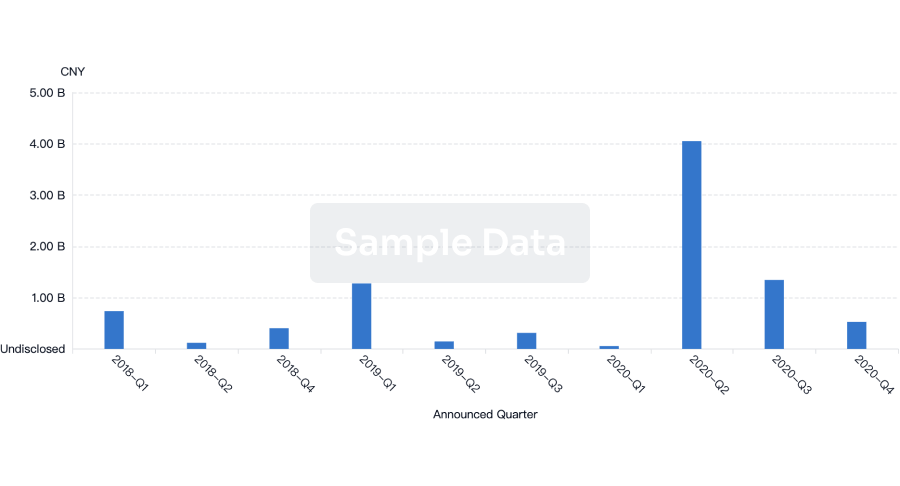
Financing
Unearth financing trends to validate and advance investment opportunities.
login
or
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free