Request Demo
Last update 01 Nov 2024

China Medical University
Last update 01 Nov 2024
Overview
Tags
Neoplasms
Other Diseases
Immune System Diseases
Small molecule drug
Disease domain score
A glimpse into the focused therapeutic areas
No Data
Technology Platform
Most used technologies in drug development
No Data
Targets
Most frequently developed targets
No Data
| Disease Domain | Count |
|---|---|
| Neoplasms | 3 |
| Hemic and Lymphatic Diseases | 1 |
| Infectious Diseases | 1 |
| Immune System Diseases | 1 |
| Top 5 Drug Type | Count |
|---|---|
| Small molecule drug | 5 |
Related
6
Drugs associated with China Medical UniversityTarget |
Mechanism Nav1.5 blockers |
Active Org. |
Originator Org. |
Active Indication |
Inactive Indication- |
Drug Highest PhaseApproved |
First Approval Ctry. / Loc. United States |
First Approval Date19 Jun 1990 |
Target |
Mechanism p38 MAPK stimulants |
Active Org. |
Originator Org. |
Active Indication |
Inactive Indication- |
Drug Highest PhasePreclinical |
First Approval Ctry. / Loc.- |
First Approval Date- |
Target- |
Mechanism Apoptosis inducers |
Active Org. |
Originator Org. |
Active Indication |
Inactive Indication- |
Drug Highest PhasePreclinical |
First Approval Ctry. / Loc.- |
First Approval Date- |
122
Clinical Trials associated with China Medical UniversityNCT06666166
Exploratory Clinical Study of SHR-A1811 Combined with Apatinib in the Treatment of Advanced Gastric or Gastroesophageal Junction Adenocarcinoma and Colorectal Cancer
To evaluate the effectiveness and safety of SHR-A1811 combined with apatinib in the treatment of advanced gastric or gastroesophageal junction adenocarcinoma and colorectal cancer.
Start Date01 Dec 2024 |
Sponsor / Collaborator |
NCT06595043
Effects of Different Occlusion Angles of Disposable Tracheal Blocker on Right One-lung Ventilation: a Multi-center, Prospective, Randomized Controlled Trial
This trial is a practical, multicenter, prospective, parallel grouping, randomized controlled,two-arm study. This study will be conducted in three centers including the First Hospital of China Medical University, Seoul National University Hospital and the University Clinical Center of Serbia. The investigators aim to investigate the effect of different occlusion angles of disposable tracheal blocker on right one-lung ventilation
Start Date09 Oct 2024 |
Sponsor / Collaborator |
NCT06604221
The Impact of Resistance Exercise on Symptom Burden in Older Patients Undergoing Maintenance Hemodialysis
The goal of this clinical trial is to learn if an intradialytic resistance exercise intervention works to reduce the symptom burden in older maintenance hemodialysis patients. It will also learn about safety of the intradialytic resistance exercise intervention program. The main questions it aims to answer are:
1. Does intradialytic resistance exercise effectively improve the number, frequency, and severity of symptoms in older patients?
2. What adverse events may occur among older dialysis patients during exercise?
Researchers will compare older dialysis patients who undergo the intradialytic resistance exercise intervention with those receiving standard care to observe whether resistance exercise can improve symptom burden.
Participants will:
1. Take an intradialytic resistance exercise intervention program developed through joint decision-making by rehabilitation experts, dialysis center physicians, nurses, and patients, conducted three times a week for 20 minutes each session, over a duration of three months.
2. Visit the hospital a monthly for texts and examinations.
3. Keep a diary of the types and frequency of adverse events during and after the exercise sessions.
1. Does intradialytic resistance exercise effectively improve the number, frequency, and severity of symptoms in older patients?
2. What adverse events may occur among older dialysis patients during exercise?
Researchers will compare older dialysis patients who undergo the intradialytic resistance exercise intervention with those receiving standard care to observe whether resistance exercise can improve symptom burden.
Participants will:
1. Take an intradialytic resistance exercise intervention program developed through joint decision-making by rehabilitation experts, dialysis center physicians, nurses, and patients, conducted three times a week for 20 minutes each session, over a duration of three months.
2. Visit the hospital a monthly for texts and examinations.
3. Keep a diary of the types and frequency of adverse events during and after the exercise sessions.
Start Date03 Oct 2024 |
Sponsor / Collaborator |
100 Clinical Results associated with China Medical University
Login to view more data
0 Patents (Medical) associated with China Medical University
Login to view more data
57,129
Literatures (Medical) associated with China Medical University01 Jun 2025·Neural Regeneration Research
Decline and fall of aging astrocytes: the human perspective
Article
Author: Semyanov, Alexey ; Verkhratsky, Alexei
01 Jan 2025·Journal of Ethnopharmacology
Periostracum Cicadae exhibits immunosuppressive effects on dendritic cells and contact hypersensitivity responses
Article
Author: Chuang, Cheng-Hsuan ; Lin, Wen-Hsin ; Chen, Chao-Jung ; Chen, Pin-Wen ; Lee, Meng-Shiou ; Lin, Ming-Kuem ; Chang, Wen-Te
01 Jan 2025·Journal of Ethnopharmacology
Engeletin attenuates the inflammatory response via inhibiting TLR4-NFκB signaling pathway in Crohn's disease-like colitis
Article
Author: Cui, He ; Shu, Chang ; Ni, Xiao ; Peng, Yuxuan ; Li, Yunwei ; Liu, Jieyu ; Wei, Ziyun
3
News (Medical) associated with China Medical University31 Dec 2022
Using AI to Fight Drug-Resistant Infections Is One of The Key Attractions
TAICHUNG,Taiwan, Dec. 31, 2022 /PRNewswire/ -- In the 2022 Healthcare+ Expo, one of the largest international healthcare fairs in Taiwan, was being held at the Nangang Exhibition Center in December. Of note was the exhibition from Taichung's China Medical University and its related healthcare system. It showed off innovations reflecting six major themes including artificial intelligence and smart medical care. Overall, the university has won 22 national awards for innovation, the highest number in Taiwan. Among them is a big data platform that utilizes environmental and clinical data from over 3 million people, and a smart anti-germ platform that can effectively combat super viruses in hospitals and also save patients from septicemia. So far, it has served more than 100,000 people. Cho Der-yang, Superintendent of China Medical University," It can take as little as one hour to know what kind of bacteria it is, and then whether there is any drug resistance, and then offer assistance in determining which medicine is most appropriate to use." The university will promote its findings and inventions in the 18 nations that are part of the government's New Southbound Policy so that the world can see Taiwan's innovative capabilities. The university will promote its findings and inventions in the 18 nations that are part of the government's New Southbound Policy so that the world can see Taiwan's innovative capabilities.
Continue Reading
In the news video of Formosa TV, Taiwan's broadcast news station, the booth from China Medical University and its related healthcare system at the 2022 Healthcare+ Expo showed off a number of achievements related to innovation and award-winning products. Wong Chi-huey, the head of the Institute for Biotechnology and Medicine Industry, was among many drawn by the exhibits. This year in 2022, China Medical University focused on six themes, including AI, smart medical care and regenerative medicine. The university has won 22 national awards for innovation, the highest number ever.
The CMUH's AI healthcare system also demonstrated how AI can save lives in ambulances. A medical personnel put a patch on a patient's chest and installed a special instrument. An electrocardiogram can be performed directly on a smart phone via Bluetooth. The CMUH has developed a heart attack remote diagnosis system using AI, which greatly shortens the process of patient checkups upon arrival at hospitals. It's already used by ambulance staff for 14 fire brigades in Taiwan's Central cities, including Taichung and Nantou.
Superintendent of China Medical University, Cho Der-yang said ,"Ambulance personnel are not doctors, so it is difficult for them to judge whether it is a myocardial infarction. This takes up a lot of time and can be shortened. You can know just after a minute after the patient's in whether there is or isn't a myocardial infarction." China Medical University has invested in a number of research and development projects. The UMCH strives to promote its findings and inventions in the 18 nations that are part of the government's New Southbound Policy so that the world can see Taiwan's innovative capabilities.
Media Contact:
Hsieh Feng Ming, [email protected]
SOURCE China Medical University Hospital

24 Nov 2022
The study also won 2022 Future Technology Award in Taiwan.
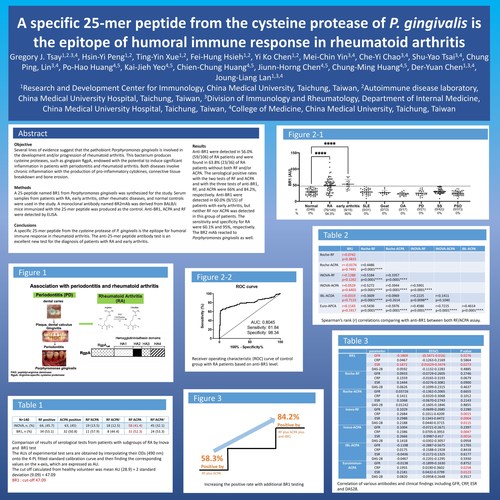
TAICHUNG,Taiwan, Nov. 24, 2022 /PRNewswire/ -- A clinical study to explore the influence of BR1 on rheumatoid arthritis conducted by Professor Gregory J. Tsai from China Medical University Hospital (CMUH) in Taiwan was published at a meeting of the American Association of Immunologist (AAI), a top medical society in the US.
Continue Reading
Figure: In 2022, Professor Gregory J. Tsay published a clinical study to explore the influence of BR1 on rheumatoid arthritis at a meeting of the American Association of Immunologists (AAI), a top medical society in US.
In the study, Dr. Gregory J. Tsay explained that rheumatoid arthritis belongs to a kind of autoimmune disease with chronic inflammation and deteriorating issues and impacts 0.5-1% of the population, Most patients are female and around 40 years old. The prevalence of arthritis in the US and China exceeds 50 million and 100 million people, respectively. The number of patients continue to grow every year. Patients usually feel joint pain, swelling, and stiffness. In particular, Dr. Gregory J. Tsay stated that many studies have indicated that rheumatoid arthritis is closely correlated with periodontal disease. The major pathogen of periodontal disease is Porphyromonas gingivalis, which generates many toxic factors, including gingipains, with many domains like RgpA (arginine gingipain) and Kpg (lysine gingipain). Therefore, the R&D team led by Dr. Gregory J. Tsay planned to determine a section of peptides for rheumatoid arthritis diagnosis in the pathogen of periodontal disease. This innovative serological target-based test has been developed as a diagnostic kit with ELISA (Anti-BR1 IgG ELISA Kit) for clinical diagnosis.
The diagnosis of rheumatoid arthritis primarily relies on two serological tests of "rheumatoid factor (RF)" and "antibody against citrullinated protein antigens (ACPA)," but no less than 30% of rheumatoid arthritis patients have negative RF or ACPA tests. Since no single test can confirm the diagnosis of rheumatoid arthritis, physicians need to combine patients' signs and symptoms, joint examination, x-rays, blood tests, etc. to rule out the diagnosis. However, physicians may be unable to prescribe the reimbursed treatments for the patients if their diagnostic test scores do not meet the criteria. Therefore, a more innovative biological labeling marker is required to improve the sensitivity of the tests and assess the treatment responses to relieve disease conditions and move toward additional treatments. In a recent case at China Medical University Hospital, Ms. Huang, a 37-year-old woman, began frequently experiencing joint redness, swelling, and pain since she was 18 years old. When she woke up in the morning, she would feel body stiffness, swelling in both knees swelling, and difficulty standing up; even her daily walking would be influenced. Because her father had a history of gout, she went to a hospital to seek help at 21 years old and was diagnosed with gout by the doctor. Afterward, she started to control her diet and undergo treatment with medication. However, she did not feel any better. By the time she was 23 years old, she visited the OPD of a well-known top physician of the Rheumatology and Immunology specialty, Professor Gregory J. Tsay. (Dr. Gregory J. Tsay) checked the patient and made an initial diagnosis ruled as rheumatoid arthritis, but both her rheumatoid factor (RF) and anti-citrullinated peptide antibodies (ACPA) tests showed negative and were unable to confirm the diagnosis. Therefore, Dr. Gregory J. Tsay's team began studying a new test for rheumatoid arthritis, which is abbreviated as the "anti-BR1 antibody test." After Ms. Huang's anti-BR1 serum test, her test results showed positive and confirmed the rheumatoid arthritis diagnosis. Ms. Huang was treated with new anti-rheumatoid drugs, including disease-modifying anti-rheumatic drugs (DMARD) and biological disease-modifying anti-rheumatic drugs (bDMARD); her joint swelling disappeared quickly, and she recovered a normal life. Currently, she maintains her treatment, and this research achievement won the honor of the 2022 Future Technology Award in Taiwan.
Precisely guided by "anti-BR1 antibody test," China Medical University Hospital (CMUH) found a method to increase 60% rheumatoid arthritis serum anti body positive rate to 80%
Dr. Gregory J. Tsay and his R&D team identified a critical section of peptides (BR1) by exploring the correlation between periodontal disease and rheumatoid arthritis to be applied to the diagnosis of rheumatoid arthritis. Through the ELISA approach, the plasma BR1 autoimmune antibody can be applied to help confirm a rheumatoid arthritis diagnosis. The team identified 76 (54.3%) rheumatoid arthritis patients with positive BR1 antibody among 140 patients with rheumatoid arthritis. One-half of the patients with negative RF and ACPA were found to have positive anti-BR1, improving the positive rate of those two traditional tests from 66.3% to 87.1%. The accuracy of the BR1 antibody test kit may elevate the sensitivity of clinical diagnosis for rheumatoid arthritis. Dr. Gregory J. Tsay further explained that the kit is expected to be the third regular test for rheumatoid arthritis diagnosis to achieve the goal of early diagnosis for subsequent early treatment; then patients can get relief from pain and improve their quality of life.
SOURCE China Medical University Hospital
Clinical ResultAACR
10 Aug 2022
A new study suggests that readily available PET scanning could enable a whole-body analysis of the effects of systemic STING-activating therapy in humans, potentially providing a diagnostic tool to guide clinical development of this treatment approach.
Stimulator of interferon genes, or STING, helps regulate immune activation. Thus, drugs that activate STING are being tested as a form of cancer immunotherapy and for treating certain infections. Findings from this study reveal previously unknown functional links between STING signaling and immunometabolism. They also suggest that positron emission tomography (PET) imaging could provide a widely accessible approach to measure the pharmacodynamic effects of using STING-activating drugs.
Oral and IV administration of STING-activating drugs stimulate potent anti-tumor responses in mouse models of cancer, suggesting this as a possible strategy for human therapy. Until now, however, researchers have not had a way to determine the magnitude, duration and location of immune activation. This research, led by UCLA Jonsson Comprehensive Cancer Center investigators, investigated whether systemic STING activation induces metabolic alterations in immune cells that can be visualized by PET imaging.
Lab mice were treated with systemic STING agonists and later imaged with PET scans using standard fluorodeoxyglucose (FDG) radiotracing. Immune cells from the spleen were analyzed by RNA sequencing and flow cytometry. The amount of tracer in B and T lymphocytes was measured. In mice bearing prostate or pancreas cancer tumors, the effects of STING agonist treatment on tracer uptake, T-lymphocyte activation marker levels, and tumor growth were evaluated.
Systemic delivery of STING-activating drugs in mice significantly increased PET tracer uptake in the spleen. Analyses of immune cells indicated an increase of tracer in both T and B lymphocytes correlated with the induction of immune cell activation markers. In tumor-bearing mice, STING agonist administration significantly delayed tumor growth and increased radiotracer uptake in secondary lymphoid glands. In addition to identifying previously unknown functional links between STING signaling and immunometabolism, the study suggests that readily available PET scanning could enable a whole-body analysis of the effects of systemic STING-activating therapy in humans. This could potentially provide a diagnostic tool guiding clinical development of this treatment approach.
"A new generation of STING agonists have broadened the available routes of administration to include systemic immune activation and are thus moving quickly in the clinical setting of cancer immunotherapy," said co-first co-author Hailey Lee, a graduate student in the laboratory of Dr. Caius Radu, a professor in the Molecular and Medical Pharmacology and Surgery Departments at UCLA and a member of the UCLA Jonsson Comprehensive Cancer Center.
Radu, the article's senior author, said, "Given that overstimulation of the immune system could lead to potential toxic side effects for STING agonists, significant questions remain in regard to optimizing the correct dose and treatment schedule for individual patients. Our recent investigation into the identification of a clinically applicable biomarker highlights PET as a readout for measuring STING agonist-induced immune activation in both the preclinical and clinical settings."
Co-first author Thuc Le, an adjunct professor of molecular and medical pharmacology at UCLA, added, "Such imaging tools can guide the dosing and scheduling of STING agonists to minimize the risk of immune overstimulation while still retaining therapeutic efficacy. We hope our findings will impact the clinical application of STING agonists."
Co-first authors Thuc Le and Hailey Lee are UCLA researchers, as are Evan Abt, Khalid Rashid, Amanda Creech, Liu Wei, Amanda Labora, Charlotte Chan, Eric Sanchez, Daniel Karin, Luyi Li, Nanping Wu, Christine Mona, Giuseppe Carlucci, Willy Hugo, Ting-Ting Wu, Timothy Donahue, Johannes Czernin, and corresponding author Caius Radu. Keke Liang is with China Medical University in Shenyang, China. Jing Cui is with Huazhong University of Science and Technology in Hubei, China. Arthur Cho is with Yonsei University College of Medicine in Seoul, South Korea. Kriti Kriti is with Elucidata Corp. in Cambridge, Massachusetts.
Immunotherapy
100 Deals associated with China Medical University
Login to view more data
100 Translational Medicine associated with China Medical University
Login to view more data
Corporation Tree
Boost your research with our corporation tree data.
login
or

Pipeline
Pipeline Snapshot as of 09 Jan 2026
The statistics for drugs in the Pipeline is the current organization and its subsidiaries are counted as organizations,Early Phase 1 is incorporated into Phase 1, Phase 1/2 is incorporated into phase 2, and phase 2/3 is incorporated into phase 3
Preclinical
4
1
Approved
Other
1
Login to view more data
Current Projects
| Drug(Targets) | Indications | Global Highest Phase |
|---|---|---|
Moricizine Hydrochloride ( Nav1.5 ) | Arrhythmias, Cardiac More | Approved |
NCKU-21 | Non-Small Cell Lung Cancer More | Preclinical |
OSU-DY7 ( p38 MAPK ) | Burkitt Lymphoma More | Preclinical |
CH-4.7 ( PD-1 ) | Neoplasms More | Preclinical |
TCH-1116 ( PKC ) | Inflammation More | Preclinical |
Login to view more data
Deal
Boost your decision using our deal data.
login
or

Translational Medicine
Boost your research with our translational medicine data.
login
or

Profit
Explore the financial positions of over 360K organizations with Synapse.
login
or

Grant & Funding(NIH)
Access more than 2 million grant and funding information to elevate your research journey.
login
or

Investment
Gain insights on the latest company investments from start-ups to established corporations.
login
or

Financing
Unearth financing trends to validate and advance investment opportunities.
login
or

AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free
