Request Demo
Last update 23 Jan 2025
CD3 x IL-5Rα
Last update 23 Jan 2025
Related
1
Drugs associated with CD3 x IL-5RαTarget |
Mechanism CD3 stimulants [+1] |
Active Org.- |
Originator Org. |
Active Indication- |
Inactive Indication |
Drug Highest PhaseDiscontinued |
First Approval Ctry. / Loc.- |
First Approval Date20 Jan 1800 |
100 Clinical Results associated with CD3 x IL-5Rα
Login to view more data
100 Translational Medicine associated with CD3 x IL-5Rα
Login to view more data
0 Patents (Medical) associated with CD3 x IL-5Rα
Login to view more data
12
Literatures (Medical) associated with CD3 x IL-5Rα01 Feb 2025·Cytokine
Exogenous binding immunoglobulin protein (BiP) enhance immune regulatory phenotype in ex-vivo Mtb infected PBMCs stratified based on QuantiFERON response
Article
Author: van Rensburg, Ilana ; Malherbe, Stephanus ; Motaung, Bongani ; Loxton, Andre G ; Gutschmidt, Andrea ; Snyders, Candice
01 Jan 2024·International Immunopharmacology
Expansion of distinct peripheral blood myeloid cell subpopulations in patients with rheumatoid arthritis-associated interstitial lung disease
Article
Author: Nelson, Amy J ; May, Sara M ; Gleason, Angela ; Romberger, Debra J ; De Graaff, Joel Van ; Schwab, Aaron ; Thiele, Geoffrey M ; Walenz, Rhonda ; Bailey, Kristina L ; Poole, Jill A ; Mikuls, Ted R ; Hershberger, Daniel ; Kramer, Bridget ; Cole, Kathryn E ; Talmadge, James E ; England, Bryant R ; Duryee, Michael J ; Gaurav, Rohit
01 Oct 2023·Clinical Immunology
Engineering bispecific T-cell engagers to deplete eosinophils for the treatment of severe eosinophilic asthma
Article
Author: Kim, Dae-Seong ; Kim, Yong-Sung ; Park, Hae-Sim ; Kim, Jun-Ho
Analysis
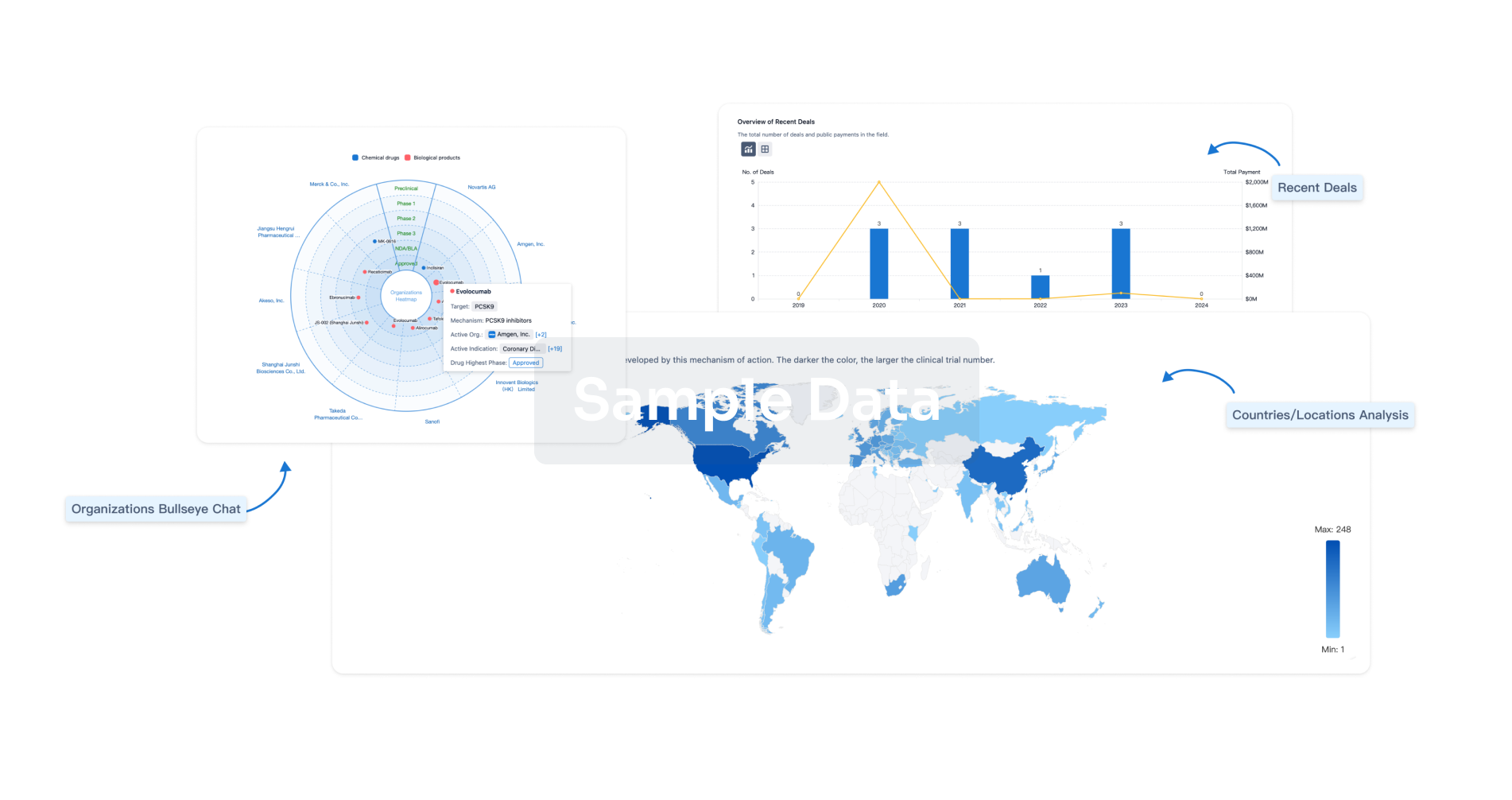
Perform a panoramic analysis of this field.
login
or
Chat with Hiro
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free