Request Demo
Last update 23 Jan 2025
IL-22 x IL-4Rα
Last update 23 Jan 2025
Related
1
Drugs associated with IL-22 x IL-4RαTarget |
Mechanism IL-22 modulators [+1] |
Originator Org. |
Active Indication |
Inactive Indication- |
Drug Highest PhasePreclinical |
First Approval Ctry. / Loc.- |
First Approval Date20 Jan 1800 |
100 Clinical Results associated with IL-22 x IL-4Rα
Login to view more data
100 Translational Medicine associated with IL-22 x IL-4Rα
Login to view more data
0 Patents (Medical) associated with IL-22 x IL-4Rα
Login to view more data
14
Literatures (Medical) associated with IL-22 x IL-4Rα01 Jun 2024·Allergy
Targeting IL ‐13 with tralokinumab normalizes type 2 inflammation in atopic dermatitis both early and at 2 years
Article
Author: Da Rosa, Joel Correa ; Staumont-Salle, Delphine ; Røpke, Mads ; Pauser, Sylvia ; Kabashima, Kenji ; Martel, Britta Cathrina ; Steffensen, Louise ; Nahm, Walter K ; Madsen, Daniel Elenius ; Arlert, Petra ; Blauvelt, Andrew ; Guttman-Yassky, Emma ; Reich, Kristian
01 Jan 2022·Molecular TherapyQ1 · MEDICINE
IL-6-elafin genetically modified macrophages as a lung immunotherapeutic strategy against Pseudomonas aeruginosa infections
Q1 · MEDICINE
Article
Author: Villeret, Bérengère ; Sallenave, Jean-Michel ; Kheir, Saadé ; Garcia-Verdugo, Ignacio
01 Sep 2021·JAAD Case Reports
Relapsing-remitting multiple sclerosis arising in a patient with atopic dermatitis on dupilumab
Author: Verhave, Brendon ; Samkoff, Lawrence ; Laageide, Leah ; Looney, Richard ; Beck, Lisa
2
News (Medical) associated with IL-22 x IL-4Rα28 May 2024
Pictured: J&J's office in Madrid, Spain/iStock, BrasilNut1
Johnson & Johnson is continuing its buying activity in the skin disease space, announcing Tuesday plans to purchase Yellow Jersey Therapeutics, a subsidiary of Numab Therapeutics, and its bispecific antibody NM26 for $1.25 billion in cash.
NM26, which started Phase I dosing in 2023, is ready to enter Phase II studies and targets two pathways to treat the skin disease atopic dermatitis (AD) or eczema. The pathways are the IL-4R alpha subunit (IL-4Rα) and IL-31. Il-4Rα triggers Th2-mediated skin inflammation, while Il-31 impacts skin itching and eventual scratching that worsen the condition.
“We are committed to developing differentiated bispecifics that combine the targeting of two distinct disease-driving pathways. NM26 can potentially deliver a treatment specifically for patients with inflamed skin associated with intense itching,” David Lee, the global immunology therapeutic area head at J&J Innovative Medicine, said in a statement.
J&J contends the candidate could effectively treat other inflammatory skin diseases that involve Th2 inflammation and itching. The deal is expected to close in the second half of 2024.
Earlier this month, J&J announced it purchased biotech Proteologix and its bispecific antibody for AD for $850 million in a cash deal and a preclinical antibody. The candidate PX128 targets interleukin 13 TSLP and is in a Phase I trial for AD. The preclinical asset that J&J also scooped up in the deal, PX130, targets Il-13 and Il-22 for moderate to severe AD.
“Our goal is to deliver transformational efficacy for all patients living with immune mediated diseases like AD,” Candice Long, worldwide vice president of immunology at J&J, said in a statement. “Our investment in differentiated bispecifics is the next chapter in our impactful Immunology legacy. It reinforces our commitment to address unmet medical needs by leveraging patient insights and our deep disease expertise.”
Numab has forged partnerships with other pharmaceutical companies, such as a development and licensing agreement with Ono Pharmaceutical in March 2024 to find an immuno-oncology candidate. The Swiss biotech received CHF 258 million ($283 million) in upfront research and milestone payments in that deal. Numab has also entered into previous development agreements with Eisai and Boehringer Ingelheim.
Tyler Patchen is a staff writer at BioSpace. You can reach him at tyler.patchen@biospace.com. Follow him on LinkedIn.
Phase 1License out/inImmunotherapyAcquisitionPhase 2
28 May 2024
Johnson & Johnson
announced it will
acquire a subsidiary of Numab Therapeutics, in a deal valued at $1.25 billion that will grant them global rights to NM26, an investigational bispecific antibody for atopic dermatitis (AD).
NM26 is designed to target two AD pathways: the IL-4R alpha subunit and IL-31, which are associated with skin inflammation and severe itching, respectively, aiming to offer a dual-targeted approach to both inflammation and itch.
AD, also known as eczema, is most common inflammatory skin condition, affecting patients with varying symptoms and disease mechanisms. Current treatments often fall short, with around 70% of patients not achieving lasting remission.
In January of this year, J&J
agreed to acquire
Ambrx Biopharma in a next-gen ADC deal valued at about $2 billion. Just a few weeks ago, J&J announced plans to acquire Proteologix, a biotech firm specializing in bispecific antibodies for immune-mediated diseases, for up to $850 million in cash and potential milestone payments.Key to the deal are Proteologix's two portfolio assets — PX128, a bispecific antibody targeting IL-13 and TSLP, and PX130, targeting IL-13 and IL-22. PX128 is set to enter phase 1 development for moderate to severe AD and asthma, while PX130 is in preclinical development for AD.
Phase 1AcquisitionADCImmunotherapy
Analysis
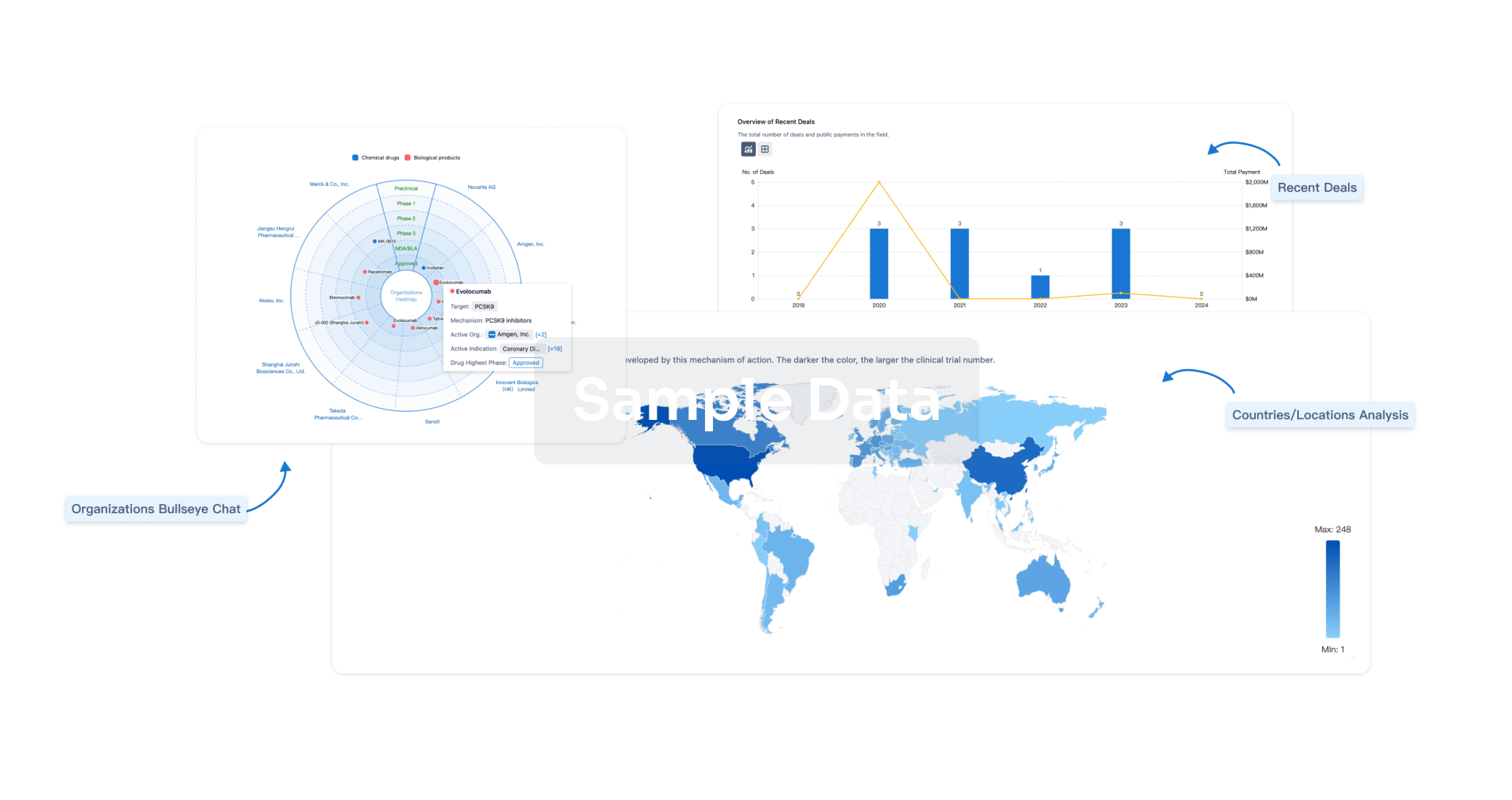
Perform a panoramic analysis of this field.
login
or
Chat with Hiro
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.
Bio
Bio Sequences Search & Analysis
Sign up for free
Chemical
Chemical Structures Search & Analysis
Sign up for free