Request Demo
What is Lenampicillin hydrochloride used for?
15 June 2024
Lenampicillin hydrochloride is a well-regarded antibiotic in the medical community, known for its efficacy against a broad spectrum of bacterial infections. Marketed under various trade names, including "Lena," "Ampilen," and "Penlen," this drug primarily targets bacterial pathogens responsible for conditions like respiratory tract infections, urinary tract infections, skin infections, and gastrointestinal infections. Developed through extensive research by numerous pharmaceutical companies and academic institutions, Lenampicillin hydrochloride belongs to the beta-lactam class of antibiotics, specifically the penicillin group. Its indications include treating infections caused by susceptible strains of bacteria, and the drug has undergone rigorous clinical trials to validate its effectiveness, safety, and therapeutic potential.
The mechanism of action of Lenampicillin hydrochloride is akin to that of other beta-lactam antibiotics. It works by inhibiting the synthesis of the bacterial cell wall, which is critical for bacterial growth and survival. The drug achieves this by binding to specific penicillin-binding proteins (PBPs) located inside the bacterial cell wall. These PBPs are enzymes involved in the final stages of synthesizing peptidoglycan, an essential component of the bacterial cell wall. By interrupting this process, Lenampicillin hydrochloride ultimately leads to cell lysis and death of the bacterium. This bactericidal action makes it highly effective in treating a variety of infections caused by Gram-positive and Gram-negative bacteria.
Administering Lenampicillin hydrochloride is straightforward, and it is available in multiple forms, including oral tablets, capsules, and injectable solutions. The method of administration largely depends on the nature and severity of the infection being treated. For instance, oral forms are generally prescribed for mild to moderate infections, while intravenous administration may be reserved for more severe cases or those requiring rapid intervention. The onset of action for Lenampicillin hydrochloride is relatively quick, with therapeutic levels achieved within one to two hours after oral ingestion. This rapid onset is beneficial for patients needing prompt relief from bacterial infections. The recommended dosage and duration of treatment vary based on the specific infection, patient age, weight, and renal function. Healthcare providers typically follow established guidelines to determine the optimal dosing regimen to maximize therapeutic outcomes while minimizing potential side effects.
Like all medications, Lenampicillin hydrochloride is not without its side effects. The most commonly reported adverse effects include gastrointestinal disturbances such as nausea, vomiting, diarrhea, and abdominal pain. These symptoms are usually mild and transient, resolving without the need for medical intervention. However, there are more serious side effects that patients should be aware of, including hypersensitivity reactions like skin rashes, itching, and in rare cases, anaphylaxis. Patients with a known allergy to penicillin or other beta-lactam antibiotics should avoid using Lenampicillin hydrochloride, as they are at a higher risk of experiencing severe allergic reactions. Additionally, prolonged use of the drug may lead to the development of antibiotic-resistant bacteria or superinfections, underscoring the importance of adhering to prescribed treatment durations. Other less common side effects include transient liver enzyme elevations, hematologic changes like leukopenia and thrombocytopenia, and neurotoxicity, particularly in patients with renal impairment.
The potential for drug interactions is an important consideration when prescribing Lenampicillin hydrochloride. Several medications can affect its efficacy or increase the risk of adverse effects. For instance, concurrent use of probenecid, a drug used to treat gout, can increase the plasma concentration of Lenampicillin hydrochloride by inhibiting its renal excretion. This interaction may necessitate dosage adjustments to avoid toxicity. Similarly, the co-administration of allopurinol, another gout medication, has been associated with an increased risk of skin rashes, which could complicate the clinical picture for patients on Lenampicillin hydrochloride. Additionally, the antibiotic may reduce the effectiveness of oral contraceptives, leading to an increased risk of unintended pregnancy. Patients should be advised to use additional non-hormonal contraceptive measures during treatment. Moreover, the combination of Lenampicillin hydrochloride with bacteriostatic antibiotics, such as tetracyclines or chloramphenicol, may antagonize its antibacterial effects, potentially reducing its therapeutic efficacy. Therefore, careful consideration and consultation with a healthcare provider are essential when Lenampicillin hydrochloride is prescribed alongside other medications.
In summary, Lenampicillin hydrochloride is a valuable antibiotic with a well-established efficacy and safety profile. Its mechanism of action involves disrupting bacterial cell wall synthesis, leading to effective bacterial eradication. Proper administration and adherence to recommended dosages are crucial for optimal therapeutic outcomes. While generally well-tolerated, awareness of potential side effects and drug interactions is essential to ensure patient safety. As with any medication, healthcare providers must carefully consider individual patient factors and existing medications to tailor treatment plans appropriately.
The mechanism of action of Lenampicillin hydrochloride is akin to that of other beta-lactam antibiotics. It works by inhibiting the synthesis of the bacterial cell wall, which is critical for bacterial growth and survival. The drug achieves this by binding to specific penicillin-binding proteins (PBPs) located inside the bacterial cell wall. These PBPs are enzymes involved in the final stages of synthesizing peptidoglycan, an essential component of the bacterial cell wall. By interrupting this process, Lenampicillin hydrochloride ultimately leads to cell lysis and death of the bacterium. This bactericidal action makes it highly effective in treating a variety of infections caused by Gram-positive and Gram-negative bacteria.
Administering Lenampicillin hydrochloride is straightforward, and it is available in multiple forms, including oral tablets, capsules, and injectable solutions. The method of administration largely depends on the nature and severity of the infection being treated. For instance, oral forms are generally prescribed for mild to moderate infections, while intravenous administration may be reserved for more severe cases or those requiring rapid intervention. The onset of action for Lenampicillin hydrochloride is relatively quick, with therapeutic levels achieved within one to two hours after oral ingestion. This rapid onset is beneficial for patients needing prompt relief from bacterial infections. The recommended dosage and duration of treatment vary based on the specific infection, patient age, weight, and renal function. Healthcare providers typically follow established guidelines to determine the optimal dosing regimen to maximize therapeutic outcomes while minimizing potential side effects.
Like all medications, Lenampicillin hydrochloride is not without its side effects. The most commonly reported adverse effects include gastrointestinal disturbances such as nausea, vomiting, diarrhea, and abdominal pain. These symptoms are usually mild and transient, resolving without the need for medical intervention. However, there are more serious side effects that patients should be aware of, including hypersensitivity reactions like skin rashes, itching, and in rare cases, anaphylaxis. Patients with a known allergy to penicillin or other beta-lactam antibiotics should avoid using Lenampicillin hydrochloride, as they are at a higher risk of experiencing severe allergic reactions. Additionally, prolonged use of the drug may lead to the development of antibiotic-resistant bacteria or superinfections, underscoring the importance of adhering to prescribed treatment durations. Other less common side effects include transient liver enzyme elevations, hematologic changes like leukopenia and thrombocytopenia, and neurotoxicity, particularly in patients with renal impairment.
The potential for drug interactions is an important consideration when prescribing Lenampicillin hydrochloride. Several medications can affect its efficacy or increase the risk of adverse effects. For instance, concurrent use of probenecid, a drug used to treat gout, can increase the plasma concentration of Lenampicillin hydrochloride by inhibiting its renal excretion. This interaction may necessitate dosage adjustments to avoid toxicity. Similarly, the co-administration of allopurinol, another gout medication, has been associated with an increased risk of skin rashes, which could complicate the clinical picture for patients on Lenampicillin hydrochloride. Additionally, the antibiotic may reduce the effectiveness of oral contraceptives, leading to an increased risk of unintended pregnancy. Patients should be advised to use additional non-hormonal contraceptive measures during treatment. Moreover, the combination of Lenampicillin hydrochloride with bacteriostatic antibiotics, such as tetracyclines or chloramphenicol, may antagonize its antibacterial effects, potentially reducing its therapeutic efficacy. Therefore, careful consideration and consultation with a healthcare provider are essential when Lenampicillin hydrochloride is prescribed alongside other medications.
In summary, Lenampicillin hydrochloride is a valuable antibiotic with a well-established efficacy and safety profile. Its mechanism of action involves disrupting bacterial cell wall synthesis, leading to effective bacterial eradication. Proper administration and adherence to recommended dosages are crucial for optimal therapeutic outcomes. While generally well-tolerated, awareness of potential side effects and drug interactions is essential to ensure patient safety. As with any medication, healthcare providers must carefully consider individual patient factors and existing medications to tailor treatment plans appropriately.
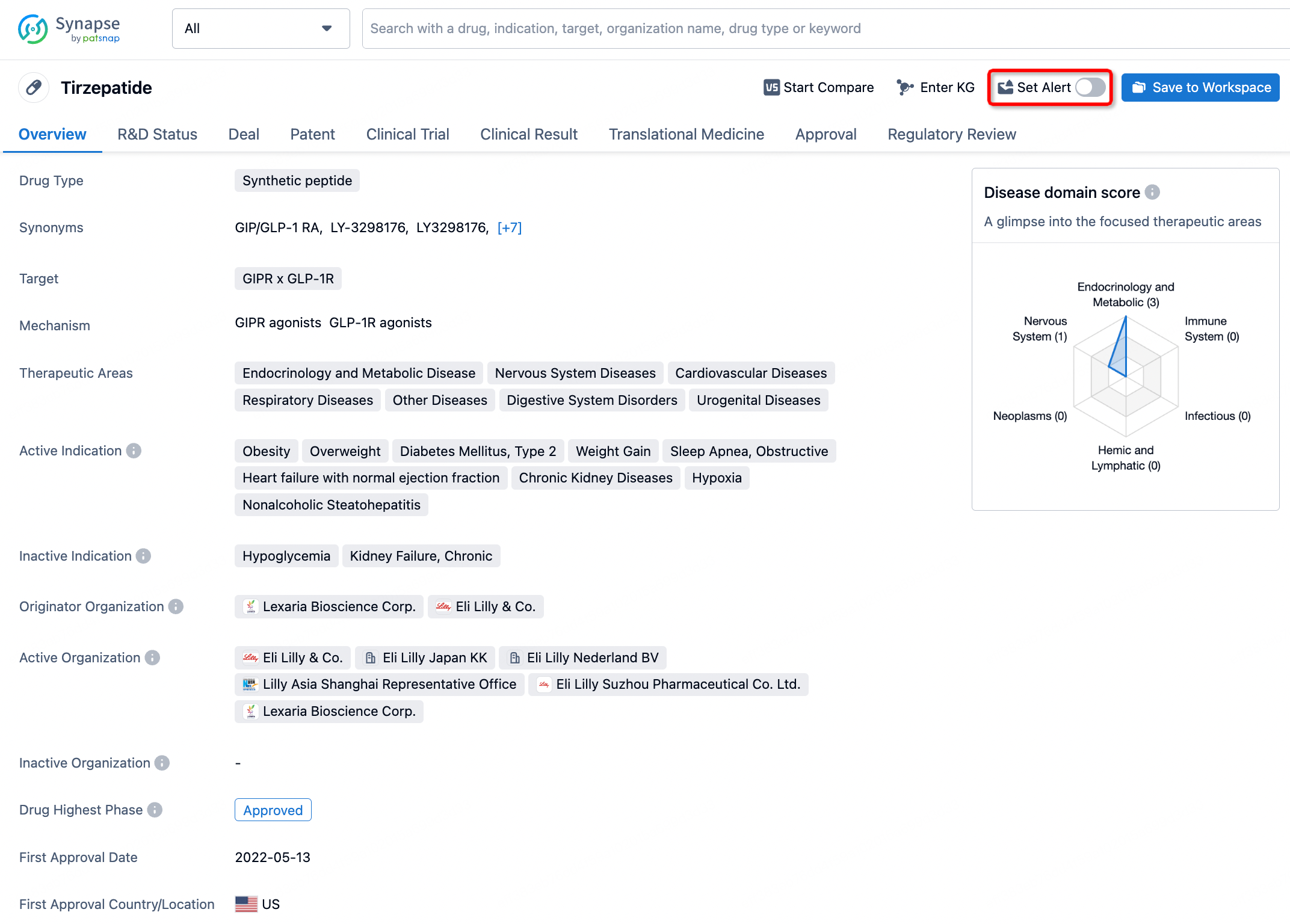
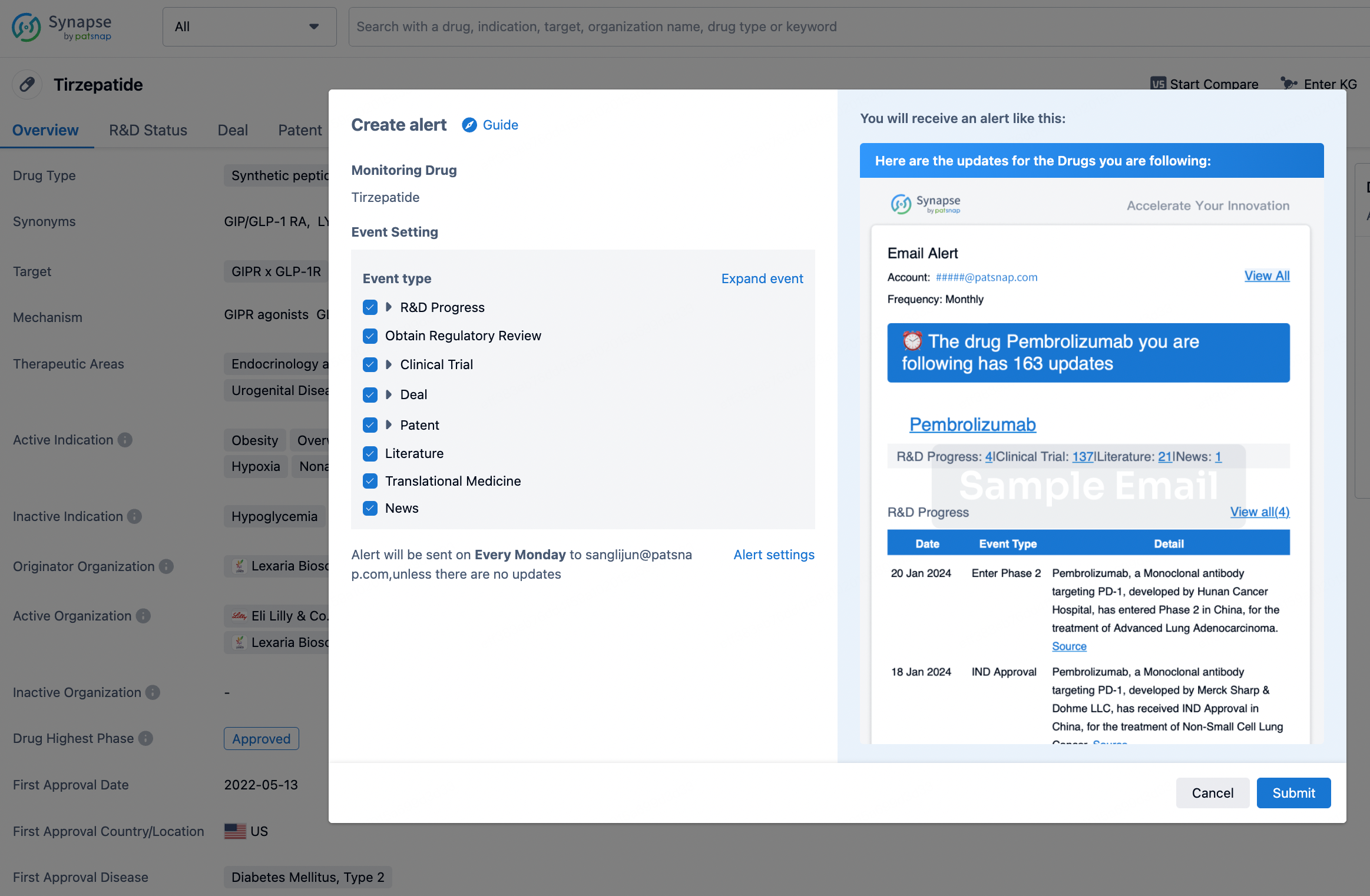
How to obtain the latest development progress of all drugs?
In the Synapse database, you can stay updated on the latest research and development advances of all drugs. This service is accessible anytime and anywhere, with updates available daily or weekly. Use the "Set Alert" function to stay informed. Click on the image below to embark on a brand new journey of drug discovery!
AI Agents Built for Biopharma Breakthroughs
Accelerate discovery. Empower decisions. Transform outcomes.
Get started for free today!
Accelerate Strategic R&D decision making with Synapse, PatSnap’s AI-powered Connected Innovation Intelligence Platform Built for Life Sciences Professionals.
Start your data trial now!
Synapse data is also accessible to external entities via APIs or data packages. Empower better decisions with the latest in pharmaceutical intelligence.