AstraZeneca's Strategic Layout for Targeting PTH1R in the Treatment of Hypoparathyroidism
On March 14th, British pharmaceutical giant AstraZeneca announced its intention to acquire Amolyt Pharma, a clinical-stage biotech company focused on the development of innovative therapies for rare endocrine diseases. The acquisition is set to further strengthen AstraZeneca's rare disease business unit, Alexion, by bolstering its late-stage product development pipeline and adding a critical component to its bone metabolism portfolio - eneboparatide (AZP-3601), a therapeutic peptide currently in phase III clinical trials. This drug has a novel mechanism of action aimed at addressing key therapeutic goals for patients with hypoparathyroidism.
It is reported that patients with hypoparathyroidism, due to insufficient production of parathyroid hormone (PTH), suffer from severe calcium and phosphate metabolism dysregulation, leading to symptoms and complications that can alter quality of life, including chronic kidney disease among others. There are an estimated 115,000 patients in the United States and about 107,000 in the European Union affected by this condition, with approximately 80% being female.
Parathyroid hormone is secreted by the four tiny parathyroid glands located near the thyroid gland. When there is an insufficiency or absence of PTH secretion, it leads to a decrease in the concentration of calcium ions in the blood and an increase in phosphate levels, which is the most significant laboratory finding for the diagnosis of hypocalcemia. The most common cause of the loss of PTH is injury or removal of the parathyroid glands during thyroid or neck surgery. This condition disrupts the normal balance of calcium and phosphate metabolism in the body, causing a range of symptoms and complications including, but not limited to, muscle cramps, twitching, tremors, fatigue, emotional instability, and potentially, if left untreated, osteomalacia, increased risk of fractures, and dental issues. Therefore, finding therapies that can substitute the function of PTH is crucial for patients with hypocalcemia, with the goal of restoring calcium-phosphate homeostasis and improving patient quality of life.

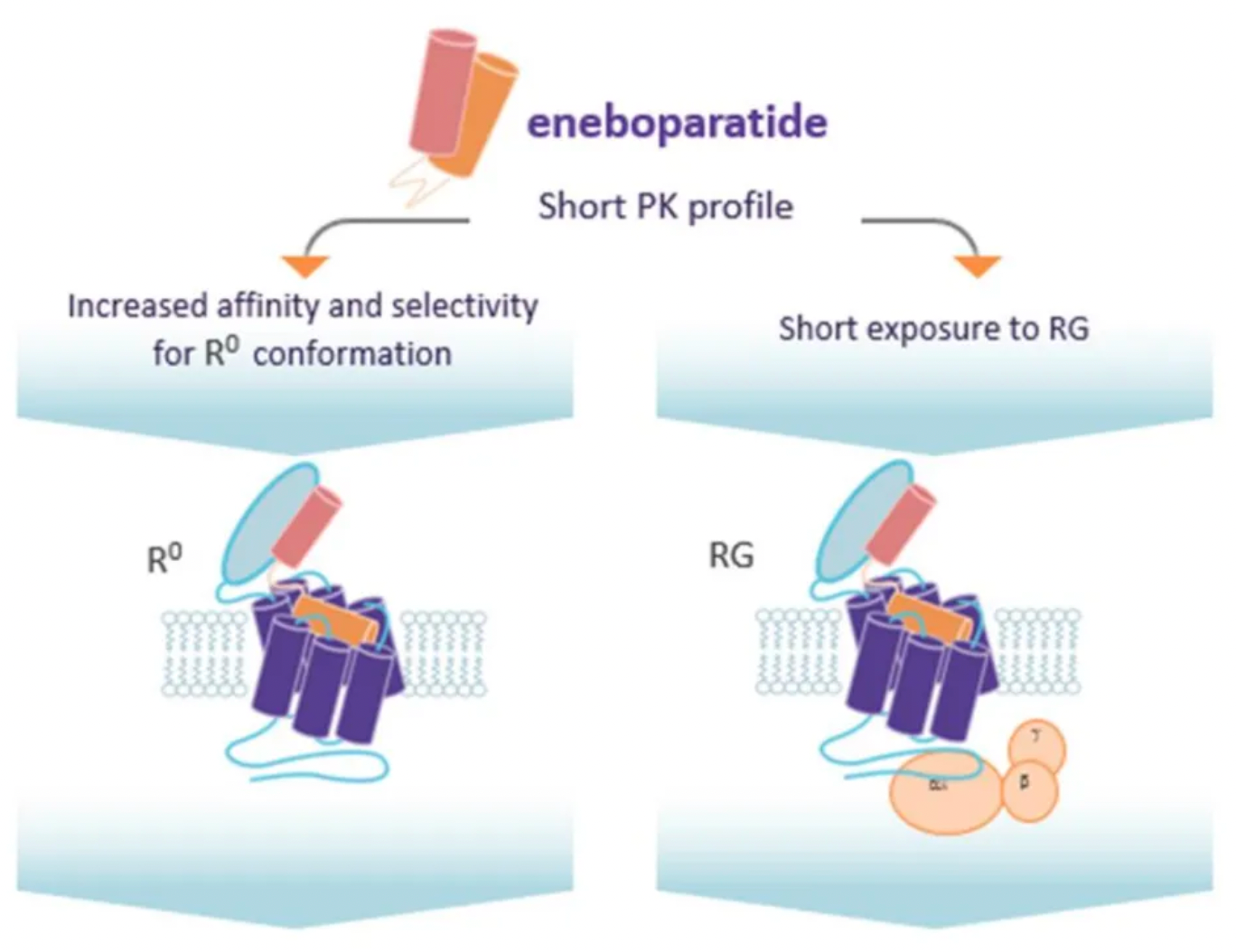
As a PTH receptor 1 (PTH1R) agonist, eneboparatide employs a novel mechanism of action specifically designed for the therapeutic aim of treating hypoparathyroidism. This peptide is capable of highly affinity binding to the R0 conformation of PTH1R receptors. Despite its short pharmacokinetic half-life, eneboparatide is still able to induce a sustained elevation in serum calcium levels in vivo. Such a design allows eneboparatide to vigorously promote calcium reabsorption in the renal tubules and exert physiologically significant effects on bone turnover, which has been confirmed by animal experiments and human studies.
In the year 2016, a research team from Harvard Medical School developed two murine models of acquired hypoparathyroidism and utilized these models to evaluate the efficacy of PTH(1-34) and a long-acting PTH analog (LA-PTH) in regulating blood calcium levels.
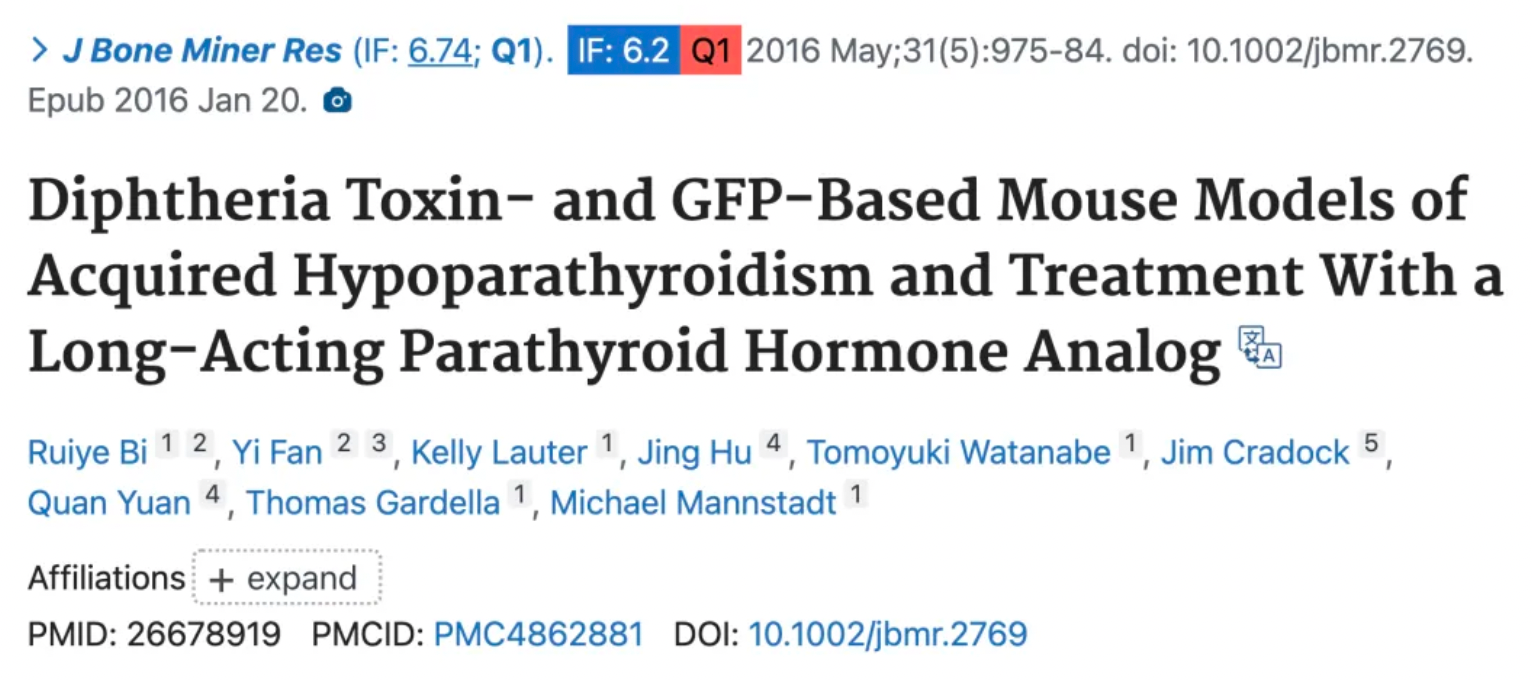
The results show that a single subcutaneous injection of LA-PTH can more effectively increase serum calcium levels compared to PTH(1-34) administered at a dose tenfold higher, with the effect lasting over 24 hours, and without leading to excessive urinary calcium excretion.
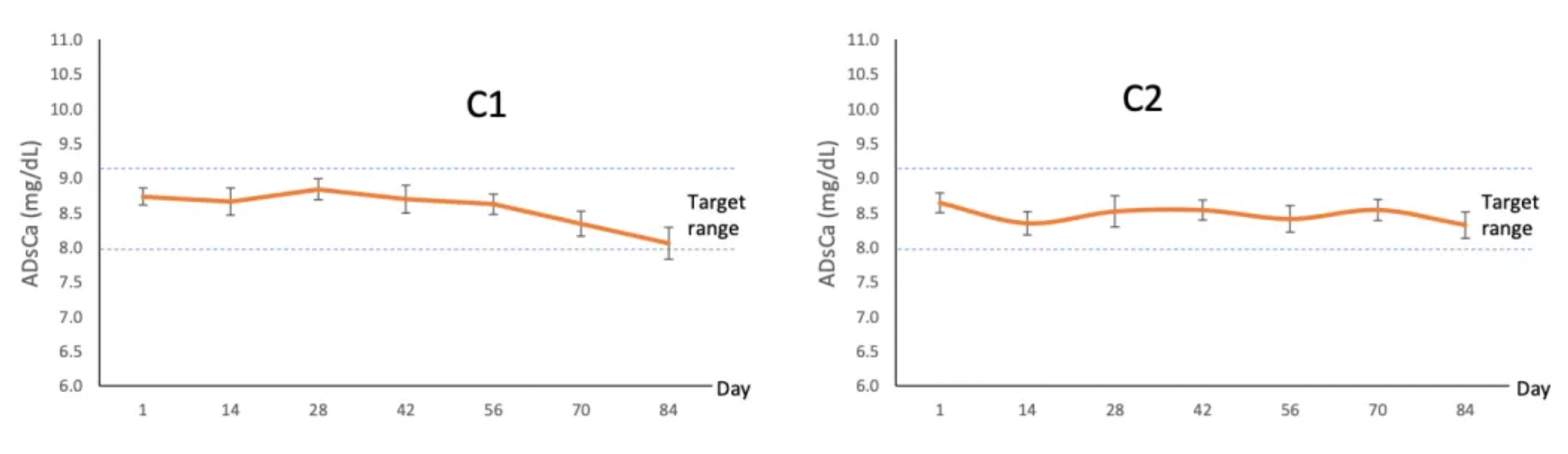
In a phase I clinical trial conducted on healthy volunteers, eneboparatide demonstrated the ability to rapidly induce a steady increase in serum calcium levels along with the dosage increment, and this elevation was maintained throughout the entire treatment period. More importantly, there was no observed increase in urinary calcium excretion during the study, nor were there any changes in bone biomarkers. This indicates that eneboparatide can raise serum calcium levels without causing negative effects on urinary calcium excretion or bone metabolism, showing good safety and potential efficacy.
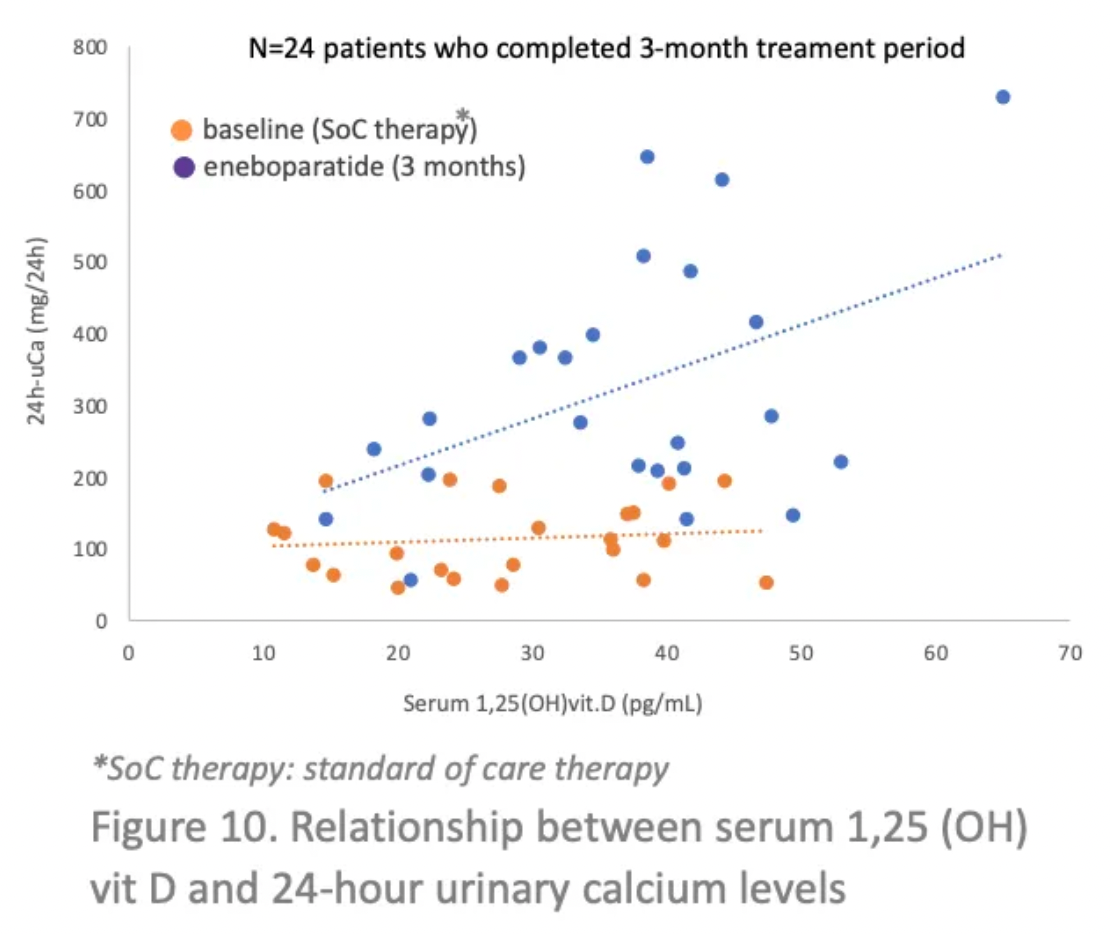

Phase II clinical data have shown that enboparatide successfully restores serum calcium levels to normal and holds promise for eliminating the patient's dependency on daily calcium and vitamin D supplements. In adults with chronic hypophosphatemia and hypercalciuria, the results indicate that enboparatide can normalize calcium content in the urine. Moreover, for patients with hypophosphatemia, enboparatide also helps maintain bone mineral density, which is a significant potential benefit for patients at increased risk of osteoporosis or reduced bone density.
About PTH1R
Currently, the main clinical targets for the treatment of hypoparathyroidism are the PTH1R (developing safer and more effective synthetic PTH analogues or oral small-molecule PTH1R agonists) and the vitamin D receptor (a type of nuclear receptor, with vitamin D receptor agonists able to control calcium and bone metabolism, and regulate growth and differentiation of various cell types).
Parathyroid hormone 1 receptor 1 (PTH1R) belongs to the Class B G protein-coupled receptor family. This receptor can be activated by two different endogenous peptide agonists, namely parathyroid hormone (PTH) and parathyroid hormone-related protein (PTHrP), leading to the activation of Gs, Gq, and β-arrestin, thereby modulating various signaling pathways and exerting different biological effects.
Research has shown that PTH can regulate the calcium and phosphate balance in bones and kidneys, while PTHrP regulates the cellular proliferation and differentiation in developing bones and other tissues. Natural PTH and modified agonist peptides can induce significant anabolic bone formation and have been used in clinical treatments for osteoporosis. Therefore, PTH1R is also considered a key target for the treatment of hypoparathyroidism and osteoporosis, and can be treated through the injection of PTH or PTHrP analogues.
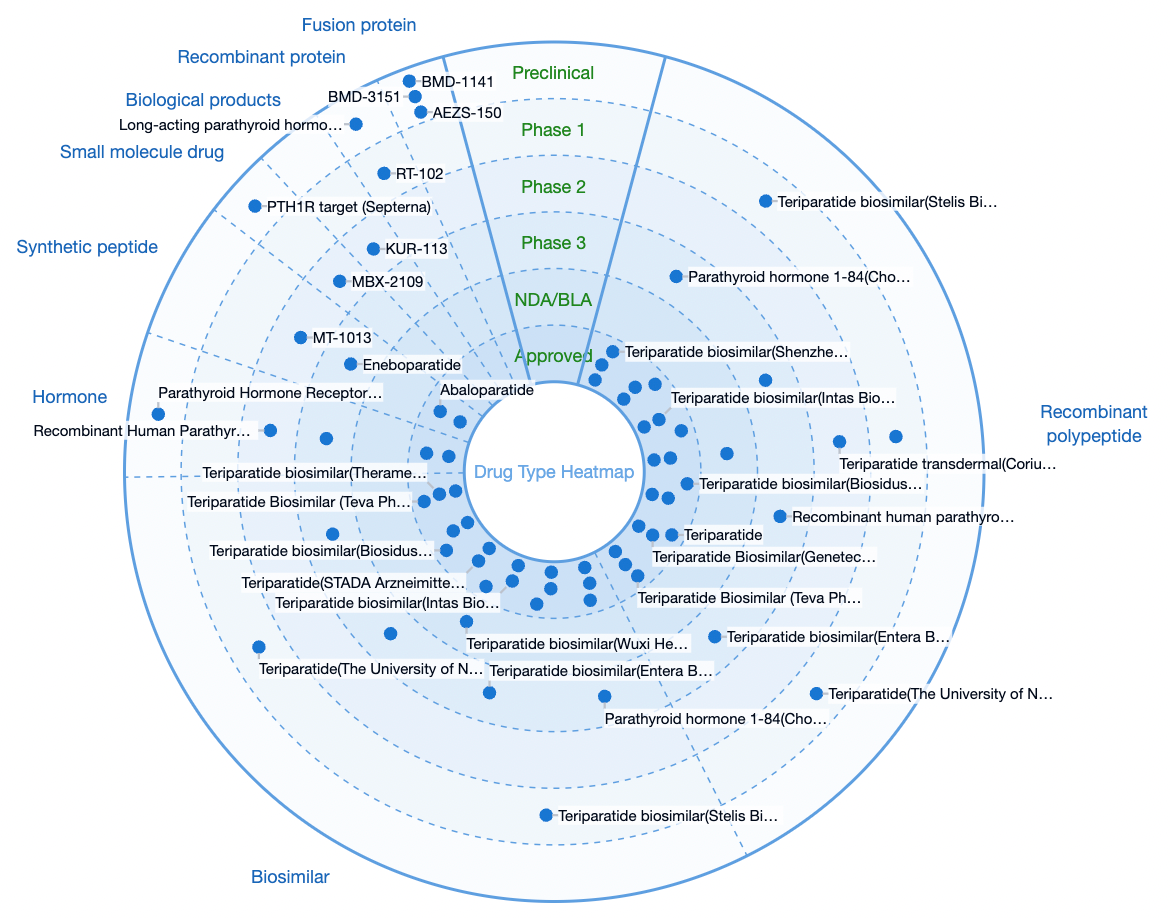
According to statistics from the Synapse database, there are currently a total of 87 therapeutic drug development projects worldwide targeting PTH1R. The types of drugs primarily consist of recombinant peptides, biosimilars, hormones, etc., with only a small portion being small-molecule drugs.
The natural ligands for Class B GPCRs are peptide hormones, which activate the receptors by binding to a larger open pocket within the transmembrane domain. Additionally, the extracellular domain is required for high-affinity ligand-receptor interactions. Therefore, drug development targeting Class B GPCRs primarily involves biologics or recombinant peptides, which is significantly different from the current market trend where drugs targeting Class A family GPCR members are mainly small molecules.
Class B GPCRs belong to the peptide hormone receptor family and are common drug targets for various metabolic disorders, including osteoporosis, Type 2 diabetes, obesity, cardiovascular diseases, and migraines. Developing oral medications targeting Class B GPCRs, to improve patient quality of life, minimize side effects, and reduce costs still poses certain challenges.
Other Drugs for the Treatment of Hypoparathyroidism
Currently, other candidate drugs targeting PTH1R for the clinical treatment of hypoparathyroidism include the PTH1R agonist PCO-371, which is developed by Chugai Pharmaceutical and is in Phase 1 clinical studies.
In 2016, Chugai Pharmaceutical published an article in the journal Nature Communications, detailing the development of an orally active small molecule PTHR1 agonist, PCO-371, for the treatment of hypoparathyroidism. PCO-371 is a novel orally active small molecule that functions as a full agonist of PTHR1. Oral administration of PCO-371 in osteoporotic rats significantly increased bone turnover rate, although the increase in bone mass was limited. In rats with hypocalcemia, PCO-371 restored serum calcium levels without increasing urinary calcium, and its effect was stronger and more sustainable than that of injected PTH. These results suggest that PCO-371 may offer a new therapeutic option for PTH-related disorders, including hypoparathyroidism.

PCO371 was obtained through cellular-level functional screening. It can stimulate COS-7 cells expressing PTH1R to produce cAMP as well as enhance the activity of phospholipase C. The action of PCO371 on PTH1R is primarily through interaction with the transmembrane region and is not affected by the receptor's extracellular domain.
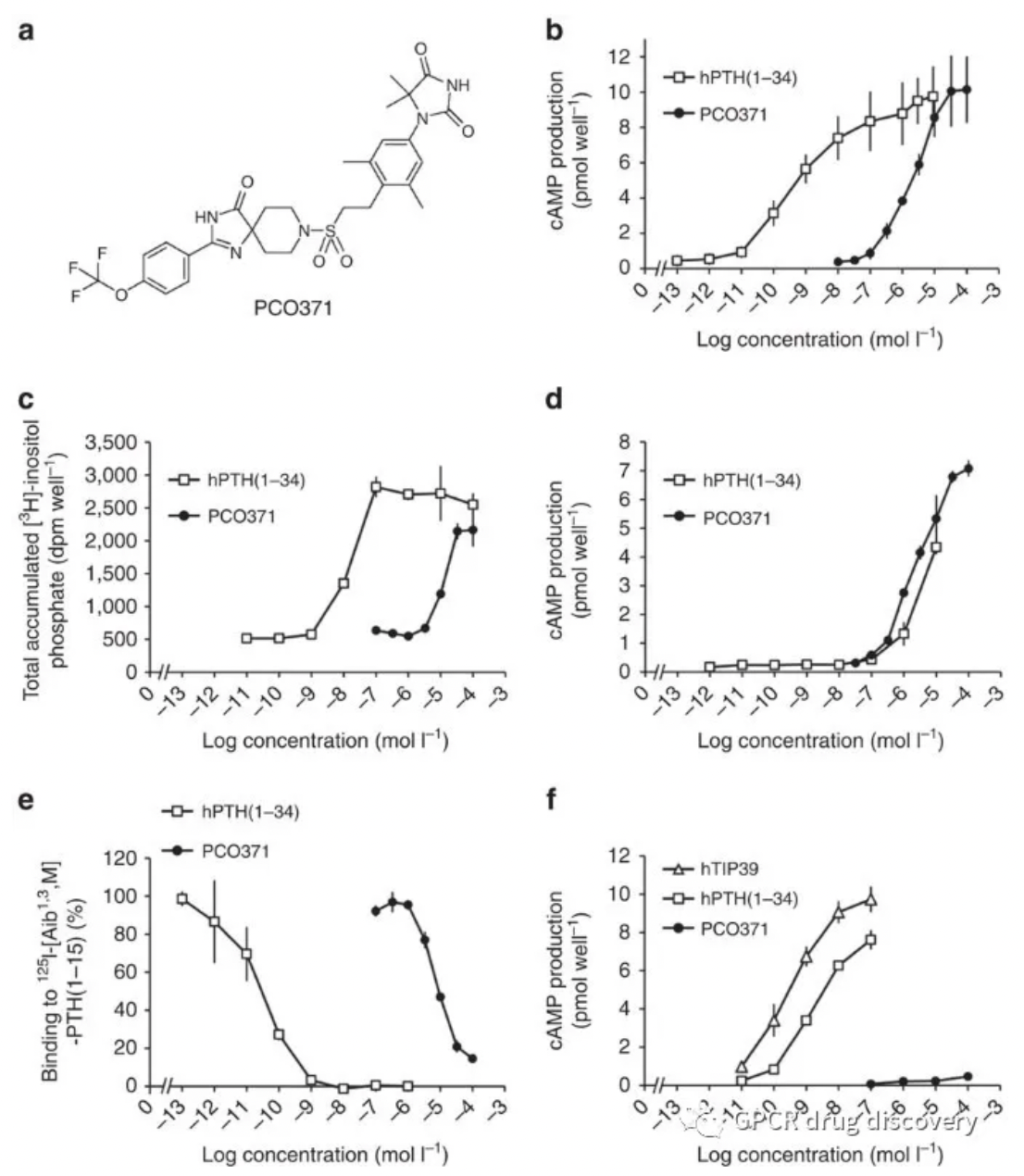
DOI: 10.1038/ncomms13384
PCO371 not only can dose-dependently increase the expression of bone-related messenger RNAs such as Fos, osteocalcin, and receptor activator of nuclear factor-κB ligand (RANKL), but it can also dose-dependently reduce the mRNA expression of osteoprotegerin and sclerostin.
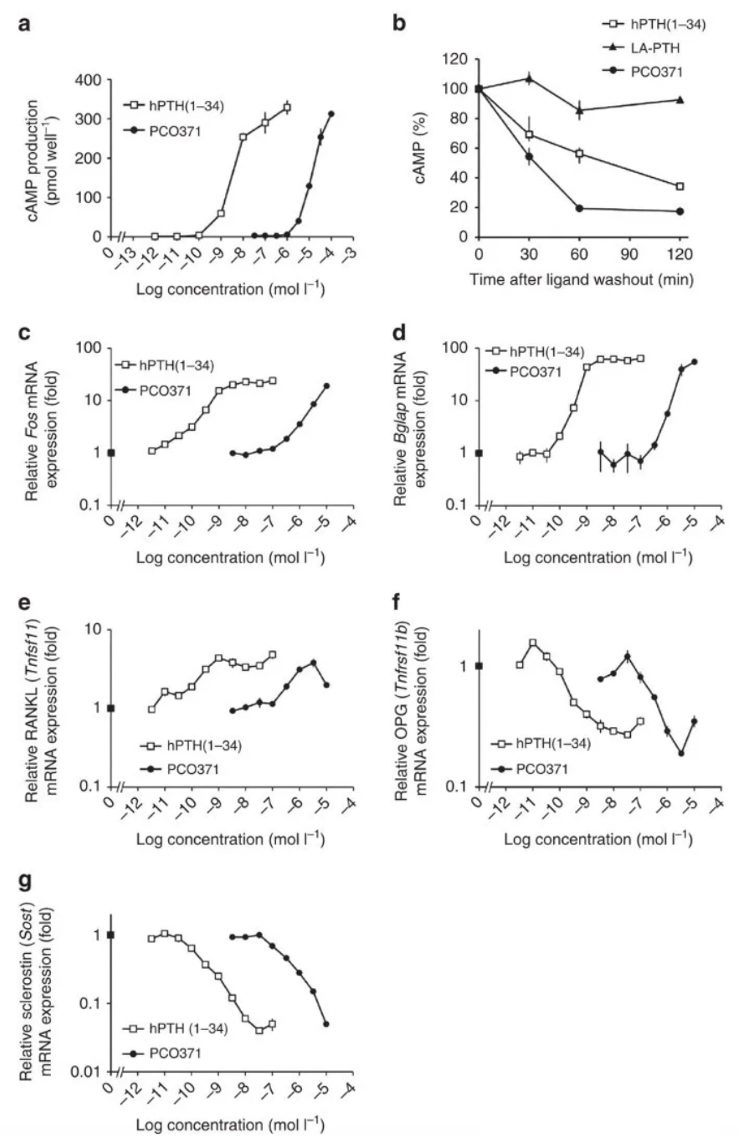
DOI: 10.1038/ncomms13384
Additionally, PCO371 is capable of inducing bone resorption activity similar to that of PTH in fetal rat long bone organ cultures. Using concentrations of 1 μmol l^-1 or higher, PCO371 stimulated the release of isotopically labeled ^45Ca from pre-labeled bone as effectively as hPTH(1-34).
Moreover, the authors investigated the effects of combined treatment with PCO371 and alfacalcidol in a hypocalcemic rat model following parathyroidectomy. Administration of 75 ng kg^-1 of alfacalcidol alone normalized serum calcium to within or above the target therapeutic range but was accompanied by substantial urinary calcium excretion. A daily oral dose of 6 mg/kg^-1 of PCO371 with 38 ng kg^-1 of alfacalcidol raised serum Ca to levels comparable to those achieved with 75 ng kg^-1 of alfacalcidol alone. The combination of PCO371 and alfacalcidol allowed for a reduction in the dose of alfacalcidol, thereby decreasing urinary calcium excretion. This suggests that PCO371 can be used in the treatment of hypoparathyroidism, either as a monotherapy or as an adjunct to conventional therapy.
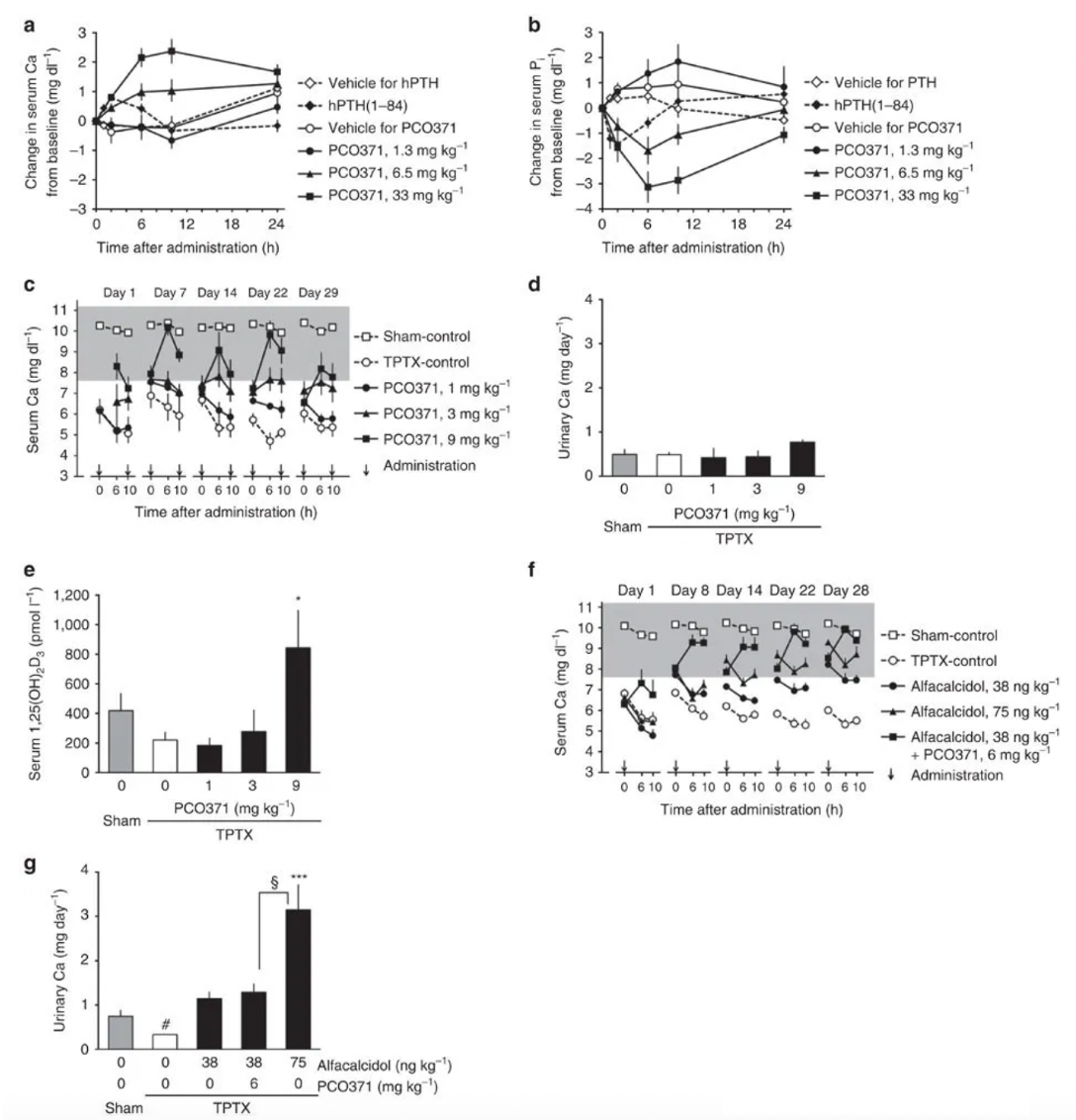
DOI: 10.1038/ncomms13384
In 2020, the Chugai team continued to publish articles in the "Journal of Medicinal Chemistry," where they discussed the small molecule hPTHR1 agonist PCO371 and its lead compound 1 (CH5447240), which could induce hypocalcemic and bile acid synthesis suppression effects similar to PTH in rats with parathyroidectomy. The compound is currently undergoing Phase I clinical trials for the treatment of hypoparathyroidism.
On December 11, Ascendis Pharma Inc. announced that the U.S. FDA had accepted the company's resubmitted New Drug Application (NDA) for palopegteriparatide (TransCon PTH) for the treatment of adult patients with hypoparathyroidism. The resubmitted application was a complete response to a Class II resubmission and set a Prescription Drug User Fee Act (PDUFA) target date of May 14, 2024.
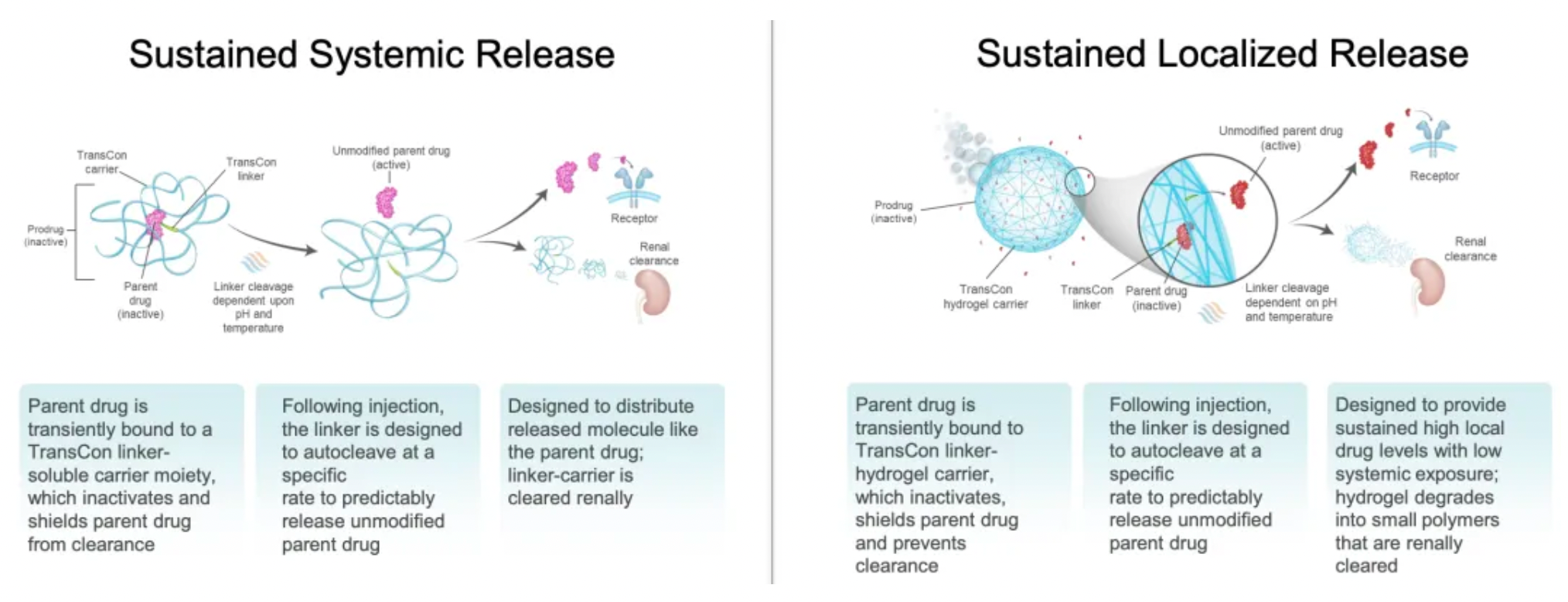
TransCon PTH is an investigational PTH hormone prodrug developed by Ascendis Pharma. It is a mPEGylated modification of the parathyroid hormone (PTH 1-34) designed for once-daily injection to provide sustained release of active PTH. The drug is currently being developed for the treatment of adult hypoparathyroidism.
Targeted PTH1R Therapy for Osteoporosis
On November 21, Apotex Inc. also announced that the U.S. FDA approved the company's Teriparatide injection for the treatment of osteoporosis. The Teriparatide injection is supplied in the form of single-patient use prefilled pens, with each pen containing 250 mcg/mL and a dosage of 20 mcg per administration.
On November 17, the U.S. FDA also approved the marketing of a Teriparatide injection by Teva Pharmaceuticals, similarly intended for the treatment of osteoporosis.
Teriparatide is a recombinant peptide and a synthetic form of natural human parathyroid hormone. This medication can help the body to form new bone, increase bone mineral density, and strengthen bones.
Abaloparatide was originally developed by Ipsen SA as an N-terminal analog of parathyroid hormone-related protein (PTHrP) and is also an agonist for the parathyroid hormone type 1 receptor (PTH1R). It is a synthetic peptide consisting of 34 amino acids and shares 41% homology with human parathyroid hormone 1-34 and human PTHrP 1-34. Following its approval in the United States in 2017, it has also been approved in countries and regions such as Japan and the European Union for the treatment of osteoporosis and postmenopausal osteoporosis.