DLL3: The Next Breakthrough in Small Cell Lung Cancer
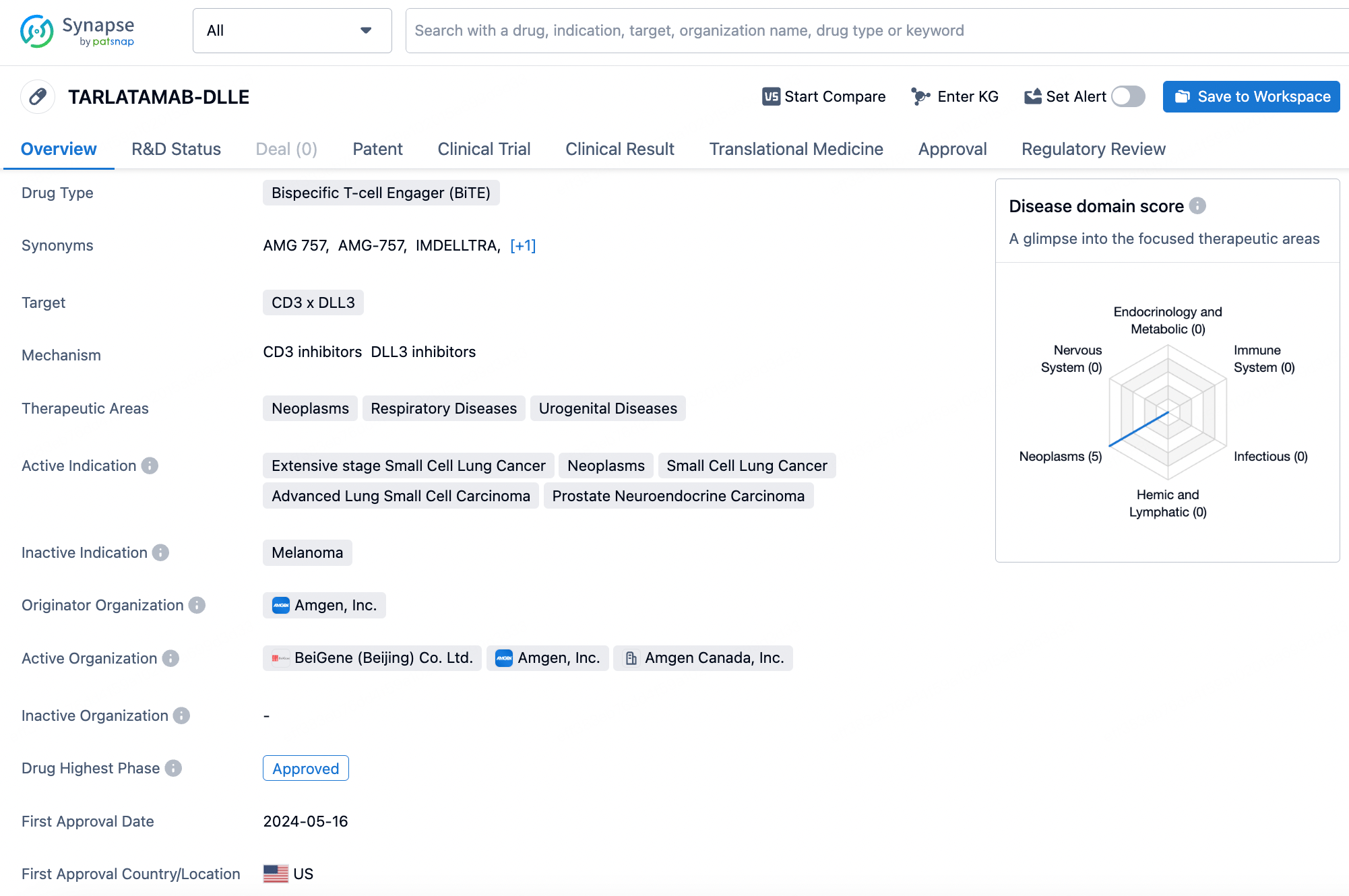
The launch of the bispecific DLL3/CD3 antibody Tarlatamab marks a significant turning point for targeting DLL3.
Prior to this, the DLL3 field was fraught with peril, exemplified by significant setbacks such as AbbVie's ADC drug Rova-T, which failed to meet PFS and OS endpoints, resulting in the termination of its development.
However, these setbacks have not dampened interest in DLL3.
In November last year, Legend Biotech and Novartis reached an agreement on the DLL3-targeted CAR-T therapy LB2102, with Legend Biotech receiving an upfront payment of $100 million and eligibility for up to $1.01 billion in potential milestone payments. In April of this year, Sino Biopharmaceutical and Boehringer Ingelheim GmbH established a strategic collaboration to develop multiple oncology products, including a DLL3/CD3 bispecific antibody.
May witnessed the market entry of Tarlatamab, achieving over $10 million in commercial revenue in its first month alone, proving to be a potent development. By August, Daiichi Sankyo announced a collaboration with Merck to co-develop the DLL-3/CD3 bispecific antibody MK-6070, acquired by Merck through the purchase of Harpoon Therapeutics for $680 million in January of this year.
Thus far, the development within the DLL3 domain has been predominantly focused on small cell lung cancer (SCLC). Why is this particular cancer type targeted? What progress can DLL3 offer? Beyond this, is there potential for other solid tumors? These are the questions that remain of keen interest.
Ideal Tumor Targets
An ideal target typically exhibits the following characteristics: high expression in tumor tissues and low expression in healthy tissues; capable of significantly promoting or supporting cellular proliferation, with cell apoptosis induced upon specific blockade. DLL3 interestingly achieves this.
DLL3 belongs to the DSL family of ligands, which bind to Notch receptors to control the Notch signaling pathway. This highly conserved signaling pathway is involved in cell proliferation, differentiation, and apoptosis. In different cellular contexts, Notch signaling can be either oncogenic or tumor-suppressive.
In normal tissues, DLL3 is characterized by low expression and is confined to the cytoplasm. However, in pathological environments, DLL3 expression not only increases but is also transported to the cell membrane. This is particularly evident in SCLC (Small Cell Lung Cancer)—clinically, DLL3 is found to be overexpressed on the cell membranes in about 80% of SCLC cases.
In the SCLC environment, Notch signaling is down-regulated. Previous reports have indicated that Notch receptors 1 and 3 play a tumor-suppressive role in SCLC. This has been supported by relevant tumor mouse models, showing that activation of Notch signaling results in decreased tumor numbers and extended survival times.
The overexpression and inhibition of DLL3 not only promote the growth of SCLC cells but also enhance their migration and invasion abilities. Additionally, it fosters resistance to platinum-based drugs through increased cell proliferation.
Furthermore, the transcription factor ASCL1, which regulates the expression of this ligand, is also a tumor-driving factor. In some SCLC cases, an increase in ASCL1 expression leads to the identification of a distinct small cell subtype, SCLC-A, suggesting that SCLC should not be viewed as a homogeneous disease.
SCLC is among the most aggressive forms of lung cancer, characterized by rapid proliferation and resistance to conventional antibiotic treatments. Over decades, the treatment modality for advanced SCLC patients has shifted, with the combined use of immune checkpoint inhibitors and chemotherapy significantly improving median survival times. However, the issue of recurrence remains unresolved, and therapeutic options for relapsed or refractory patients are extremely limited.
It can be said that SCLC is almost a chosen realm for DLL3, with pharmaceutical companies focusing their development on this target primarily within the SCLC domain.
Besides SCLC, DLL3 is also expressed in other neuroendocrine-derived tumor types, including melanoma, polymorphic glioblastoma, small cell bladder cancer, and castration-resistant prostate cancer. This also confers additional potential for DLL3.
Failures and Successes in SCLC
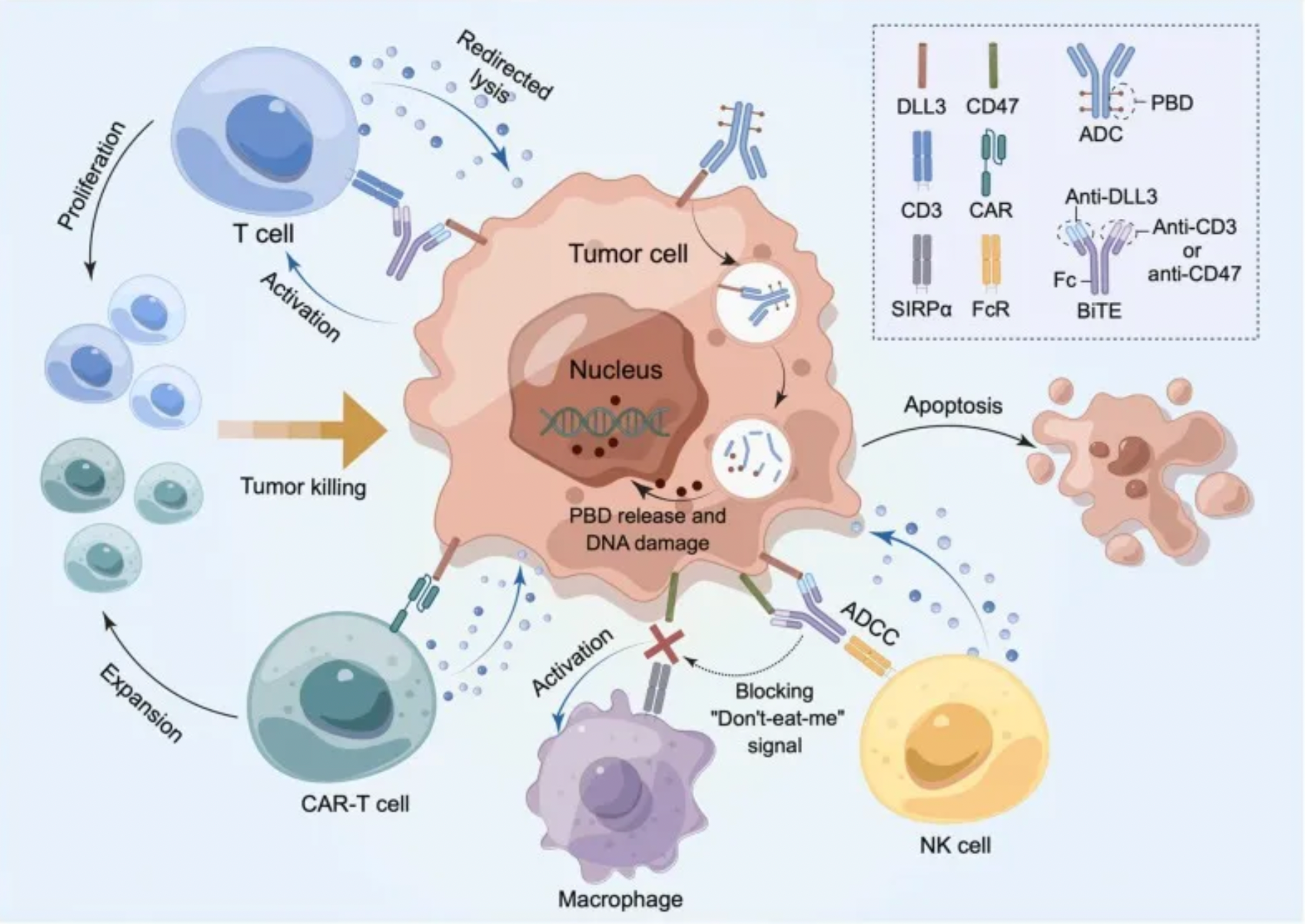
AbbVie's ADC (antibody-drug conjugate) drug Rova-T was once viewed as a beacon of hope for revolutionizing the treatment landscape of small cell lung cancer (SCLC), similar to the transformative impacts observed in breast cancer and bladder cancer. Rova-T is composed of a DLL3-targeted antibody, a linker sensitive to lysosomal enzymes, and a PBD toxin. Upon binding to DLL3 on the cell surface, Rova-T is internalized along with its receptor through endocytosis. The linker is then cleaved in the lysosome, releasing the PBD toxin into the cytosol, which subsequently enters the nucleus and crosslinks DNA, leading to cell apoptosis.
In Phase I clinical trials targeting refractory SCLC patients, Rova-T demonstrated impressive therapeutic efficacy. Initial studies in humans showed an overall response rate (ORR) of 18%, which increased to 38% in patients with high DLL3 expression in SCLC. Following these results, AbbVie initiated subsequent phases of research.
However, the outcomes were disappointing. In a Phase II study, Rova-T was examined as a third-line treatment or beyond in 339 SCLC patients expressing DLL3, achieving an ORR of only 12.4% and a median overall survival (OS) of 5.6 months. More critically, in two Phase III trials, Rova-T underperformed in head-to-head comparisons with the second-line therapy drug Topotecan, and as a maintenance therapy following first-line treatment, it was even less effective than a placebo. Consequently, AbbVie made a swift decision to cease further development of Rova-T.
The introduction of Amgen's Tarlatamab has turned the tide. Tarlatamab is a bispecific antibody targeting CD3/DLL3, simultaneously blocking the interaction between DLL3 positive tumor cells and CD3 positive T cells, inducing tumor cell redirection lysis and accompanying T cell proliferation. The phase II study, DeLLphi-301, aims to assess the anti-tumor activity, safety, side effects, and pharmacokinetics of tarlatamab in patients with advanced SCLC who have undergone two or more lines of prior treatment.
The study is divided into three parts; the first part involves dose evaluation comparison in approximately 180 patients, the second part includes patients only from the selected dose group (up to 100 patients in total from parts one and two), and the third part is a sub-study conducted after enrollment completion in part two, with the in-hospital monitoring time reduced from 48 hours post-infusion to 24 hours.
The selected standard dosage is 10 mg. In this dose group, patients with recurrent/refractory extensive-stage SCLC who progressed after platinum-based chemotherapy had an ORR of 40%, and the median DOR reached 9.7 months. Based on these results, the FDA approved Tarlatamab for market in May this year.
Diverse Drug Development
Rova-T and Tarlatamab each represent different types of drugs developed to target DLL3. Amgen's AMG 119 represents another category, that is, CAR-T therapy. The mechanism of this cell therapy involves modifying a patient's autologous T cells to express a chimeric antigen receptor (CAR) that targets DLL3, and attacks DLL3-positive cells. In preclinical studies, AMG 119 specifically lysed SCLC cell lines expressing DLL3 and inhibited tumor growth in SCLC xenograft models.
Currently, AMG 119 has achieved Phase I clinical results. Out of four evaluable patients, one experienced a confirmed partial remission at 1.1 months after the initial dosing, with a rapid decrease in total circulating tumor cell levels within seven days from the start of treatment; two patients achieved stable disease, one of whom showed a 16% reduction in target lesions compared to baseline. The median progression-free survival (PFS) was 3.7 months, and the median overall survival (OS) was 7.4 months.
Furthermore, the safety profile is manageable. Reported adverse effects include pneumonia, epilepsy, supraventricular tachycardia, and anemia. However, to date, Amgen has not provided further updates on the clinical progress of AMG 119.
Beyond antibodies, ADCs, and CAR-T, RDC (Radiolabeled Drug Conjugates) has also been introduced into the development of novel therapies targeting DLL3. RDCs aim to deliver potent radioactive elements to solid tumors with high-affinity DLL3 expression while reducing radiotoxicity to other tissues and organs. Currently, there are two investigational drugs: 89Zr-DFO-SC16.56 and ABD-147.
Apart from the diversity of drug types, indications are also being expanded. For example, Legend Biotech's CAR-T therapy LB-2102 is targeted at a broader range of neuroendocrine tumors, including not just SCLC but also large cell neuroendocrine carcinoma of the lung.
The list above is not exhaustive of all drugs under development or all potential indications. However, it highlights that the development of drugs targeting DLL3 is progressing in multiple directions, potentially bringing new possibilities to cancer treatment.
How to obtain the latest research advancements in the field of biopharmaceuticals?
In the Synapse database, you can keep abreast of the latest research and development advances in drugs, targets, indications, organizations, etc., anywhere and anytime, on a daily or weekly basis. Click on the image below to embark on a brand new journey of drug discovery!
Reference
1.Zhang H, Yang Y, Li X, Yuan X, Chu Q. Targeting the Notch signaling pathway and the Notch ligand, DLL3, in small cell lung cancer. Biomed Pharmacother. 2023;159:114248.
2.Rudin, C.M., Reck, M., Johnson, M.L. et al. Emerging therapies targeting the delta-like ligand 3 (DLL3) in small cell lung cancer. J Hematol Oncol 16, 66 (2023).
3.Ahn MJ, Cho BC, Felip E, et al. Tarlatamab for Patients with Previously Treated Small-Cell Lung Cancer. N Engl J Med. 2023;389(22):2063-2075.