Development Trends of Peptide Pharmaceuticals
Over the past year, peptide-based pharmaceuticals have garnered significant market attention. On one hand, GLP-1 peptide drugs have sparked the treatment market for obesity and metabolic diseases; on the other hand, several nuclear medicine companies, long dedicated to the development of peptide-receptor radionuclide therapy (PRRT), have been successively acquired by international pharmaceutical giants.
This article provides an interpretation of a review published in the 2021 issue of "Nature Reviews Drug Discovery", which analyzes the history and trends of peptide drug development over the past 100 years.
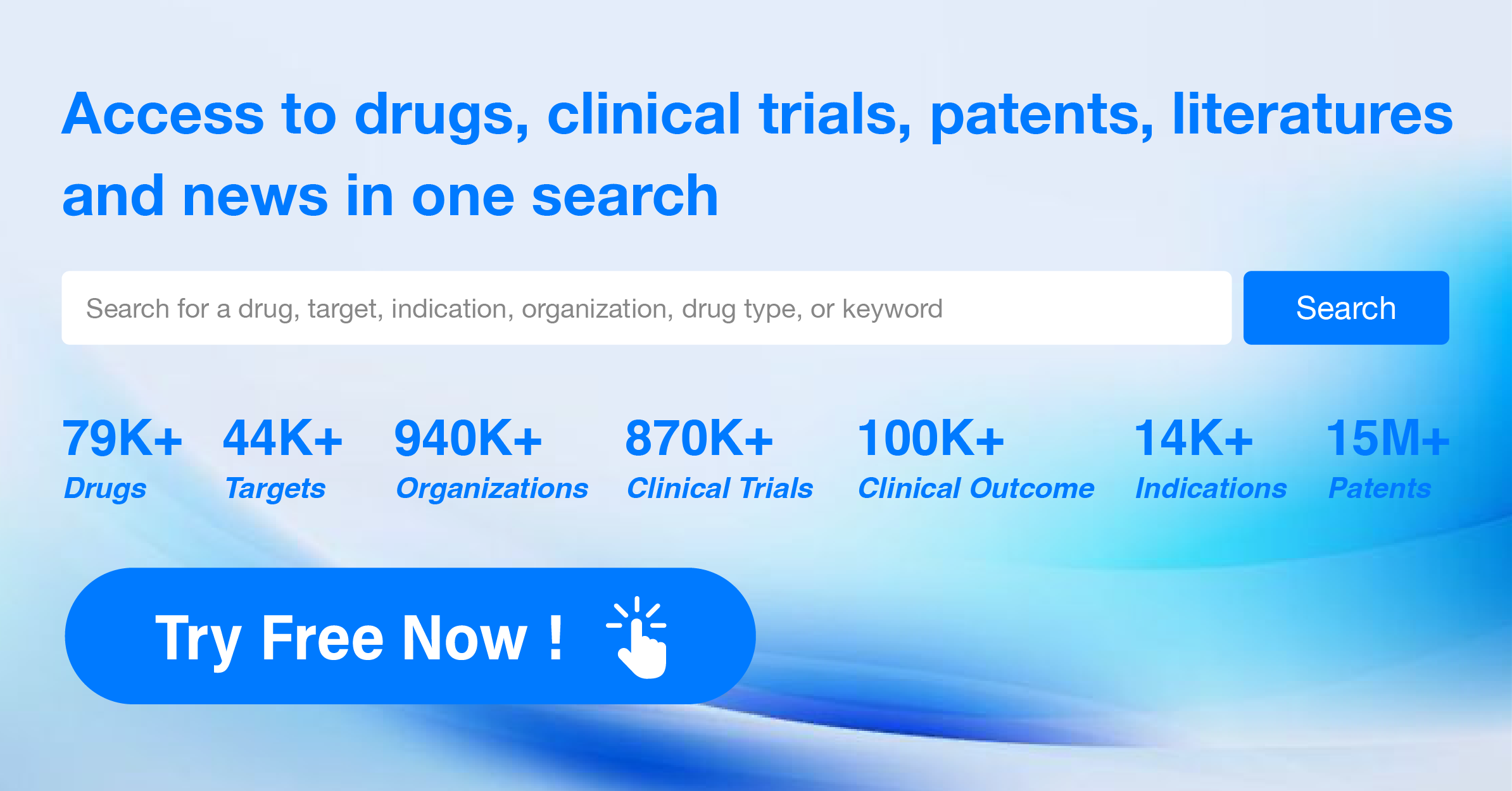
Since the first medical application of insulin in 1922, peptide drugs have played a significant role in treating a variety of diseases, including diabetes, cancer, osteoporosis, multiple sclerosis, HIV infection, and chronic pain. Currently, there are approximately 80 peptide drugs on the global market, with more than 150 in the clinical development stage, and an additional 400 to 600 undergoing preclinical research.
This article not only reviews early research methods, such as chemical modification of natural hormones like insulin to enhance their stability and pharmacological activity, which still hold important lessons for today, but also investigates emerging strategies. Venomics and peptide display libraries are among these new strategies that have opened new avenues for the discovery of peptide drugs.
Furthermore, the article analyzes areas where peptide drugs might offer unique value within the current pharmaceutical landscape, especially in therapeutic areas where traditional small molecule drugs or biologic agents are ineffective. However, to fully realize the potential of peptide drugs, a series of challenges need to be addressed, including improving oral bioavailability, enhancing plasma stability, prolonging half-life in the body, and reducing production costs.
Development in the Field of Peptide Therapeutics
The origin of peptide drugs can be traced back to the era of peptide hormones, among which insulin, as the first therapy derived from endogenous hormones, was initially extracted from the pancreases of cows and pigs, thus opening the door to peptide drug research and development.
In 1954, the research team led by Vincent du Vigneaud completed the total synthesis of oxytocin and vasopressin, and as a result, won the Nobel Prize in Chemistry in 1955. This represented a major breakthrough in the chemical synthesis of peptide compounds. In the 1950s, artificially synthesized peptide hormones such as oxytocin and vasopressin entered clinical use, and the involvement of industrial groups like Swiss companies Ciba and Sandoz further propelled the interest in and commercialization process of the peptide drug industry.
However, the efficiency of the early solution-phase chemical synthesis methods was low. It was not until the invention of solid-phase peptide synthesis technology in 1963 and its combination with high-performance liquid chromatography purification techniques that the development of peptide drugs began to attract widespread attention in the pharmaceutical industry. Bruce Merrifield proposed the concept of assembling amino acids on a solid phase to automate peptide synthesis, thereby inventing solid-phase peptide synthesis technology. This revolutionary method greatly improved the efficiency and precision of peptide synthesis and ultimately earned him the Nobel Prize in Chemistry in 1984.
As the understanding of the critical role of peptide biomediators deepens, their exceptional activity, selectivity, and low toxicity characteristics are recognized. However, the limitations of peptide drugs, including low oral bioavailability, poor plasma stability, and short in vivo half-life, are also noted.
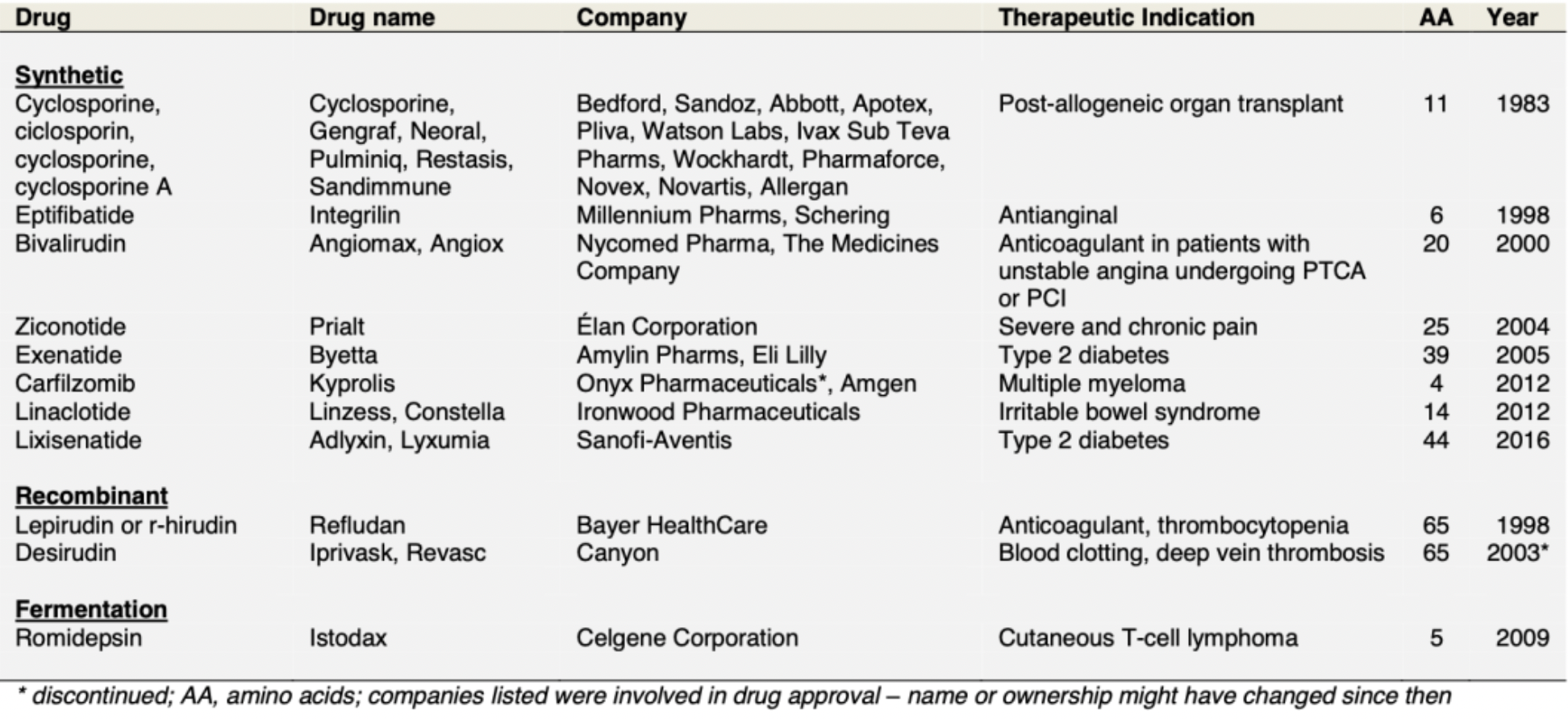
Despite this, during the golden age of small molecule drugs in the 1970s and 1980s, research on peptide drugs did not come to a halt. Instead, it progressed by continually improving drug delivery technologies, formulations, and synthesis processes, overcoming these challenges. Entering the 1980s, with the advent of recombinant technology, scientists were able to produce larger molecular weight peptides more cleanly.
In the late 1980s, with the support of venture capital and biotech companies, the development of peptide drugs witnessed a second surge. The successful commercialization of recombinant human insulin and the approval of gonadotropin-releasing hormone analogs such as leuprolide and goserelin verified the market viability of peptide drugs and spurred further investment and research activity.
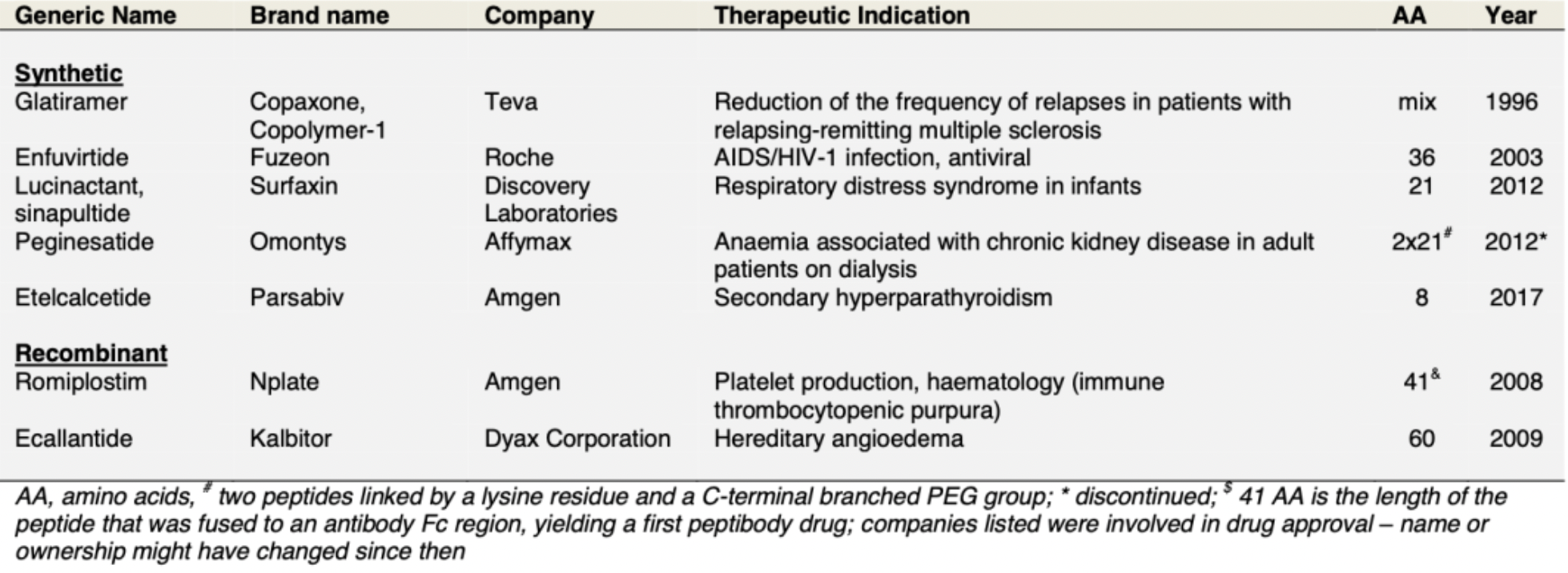
In the late 1990s, researchers adopted a series of strategies to increase the molecular weight of peptides, such as coupling peptides with lipids, larger proteins, or polyethylene glycol. These strategies effectively addressed the issue of rapid renal clearance of peptide drugs, extending their circulation time in the plasma. In addition, advancements in display technologies played a significant role; for instance, phage display technology enabled researchers to directionally discover peptide sequences with better pharmacological properties and higher drug-likeness from large-scale libraries.
As time progressed, the peptide drug market continued to expand, with approved drugs covering the treatment of various diseases such as diabetes, cancer, and osteoporosis. Moreover, through continuous technological innovation and deepening biological understanding, the research and development of peptide drugs is continuing to evolve towards greater efficiency, safety, and adaptability. From 2000 to 2010, the number of peptide drugs entering clinical trials almost doubled compared to the 1990s.
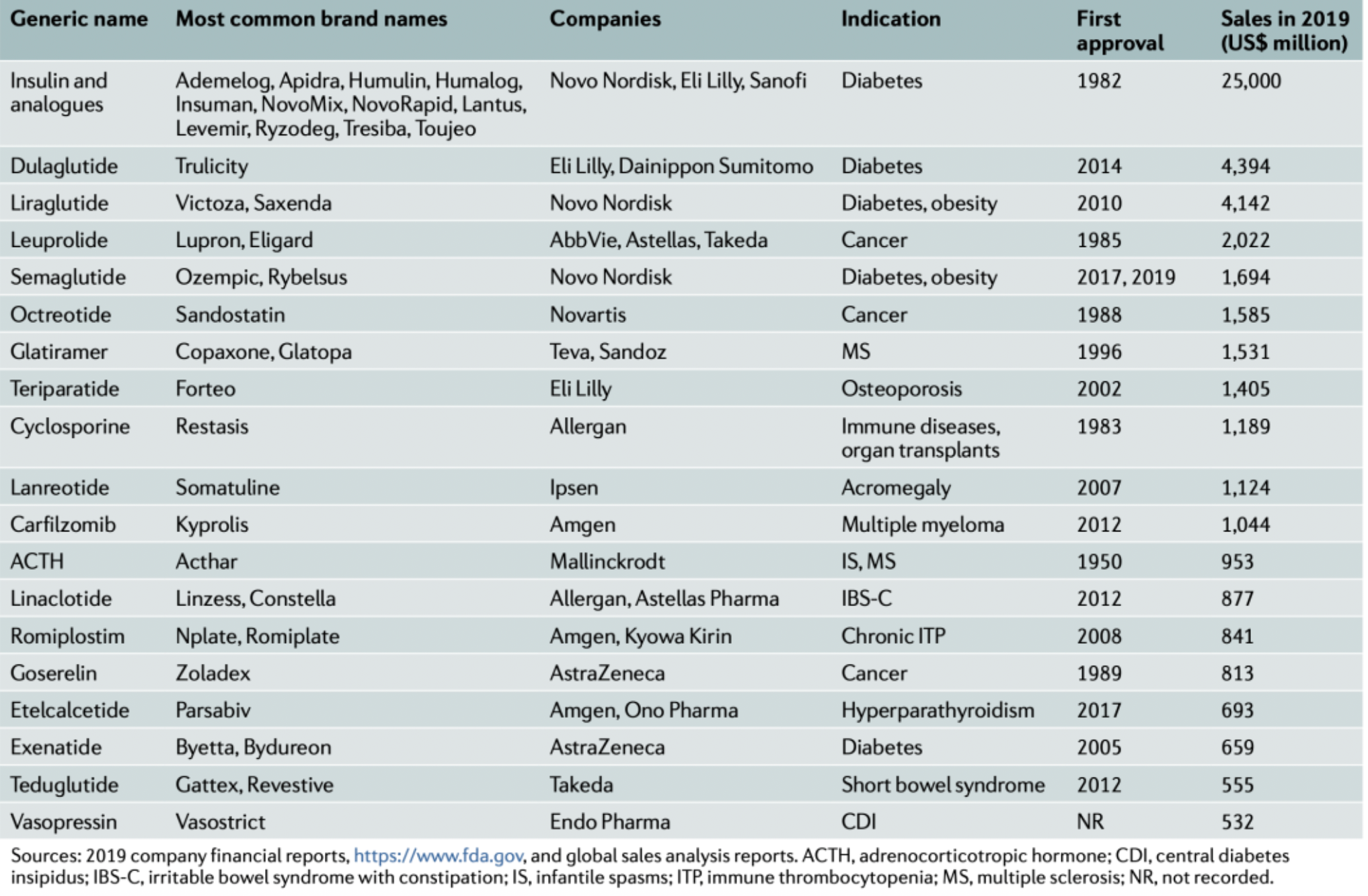
The Peptide Therapeutics Market
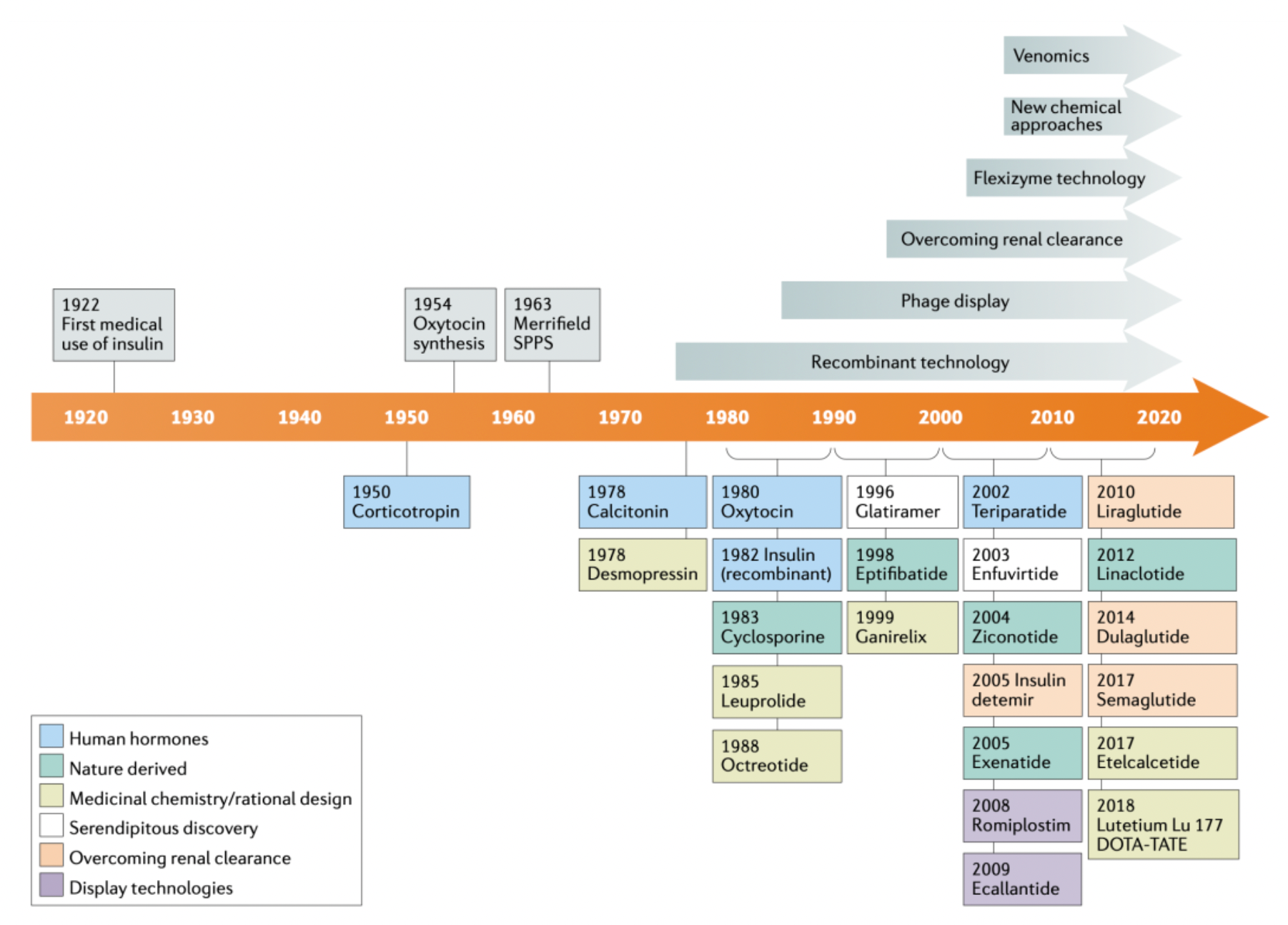
The peptide drug market occupies a unique pharmacological domain that lies between small molecule drugs and biological products. In the global pharmaceutical market, peptide drugs account for 5%, with a worldwide sales exceeding 50 billion USD in 2019. Over the past sixty years, the number of approved peptide drugs has steadily increased, with the global peptide therapeutics market experiencing an average growth rate of approximately 7.7%.
In the sales revenue of peptide-based pharmaceuticals, insulin and its analogs account for approximately half of the market share (about $25 billion), demonstrating their dominant position in the field. Following closely are a series of important peptide drug products: for instance, the GLP-1 receptor agonist dulaglutide (brand name Trulicity), which is used for diabetes treatment, achieved sales of $4.4 billion in 2019; another GLP-1 receptor agonist, liraglutide, marketed under the brands Victoza and Saxenda for diabetes and obesity treatments respectively, reached sales of $4.1 billion; and the synthetic gonadotropin-releasing hormone analog leuprorelin (brand names Lupron and Eligard), mainly used for cancer treatment, with a sales volume of $2 billion.
Based on currently approved peptide drugs, the majority are categorized as agonists, and the most frequently targeted indications are related to endocrinology, metabolism, and oncology.
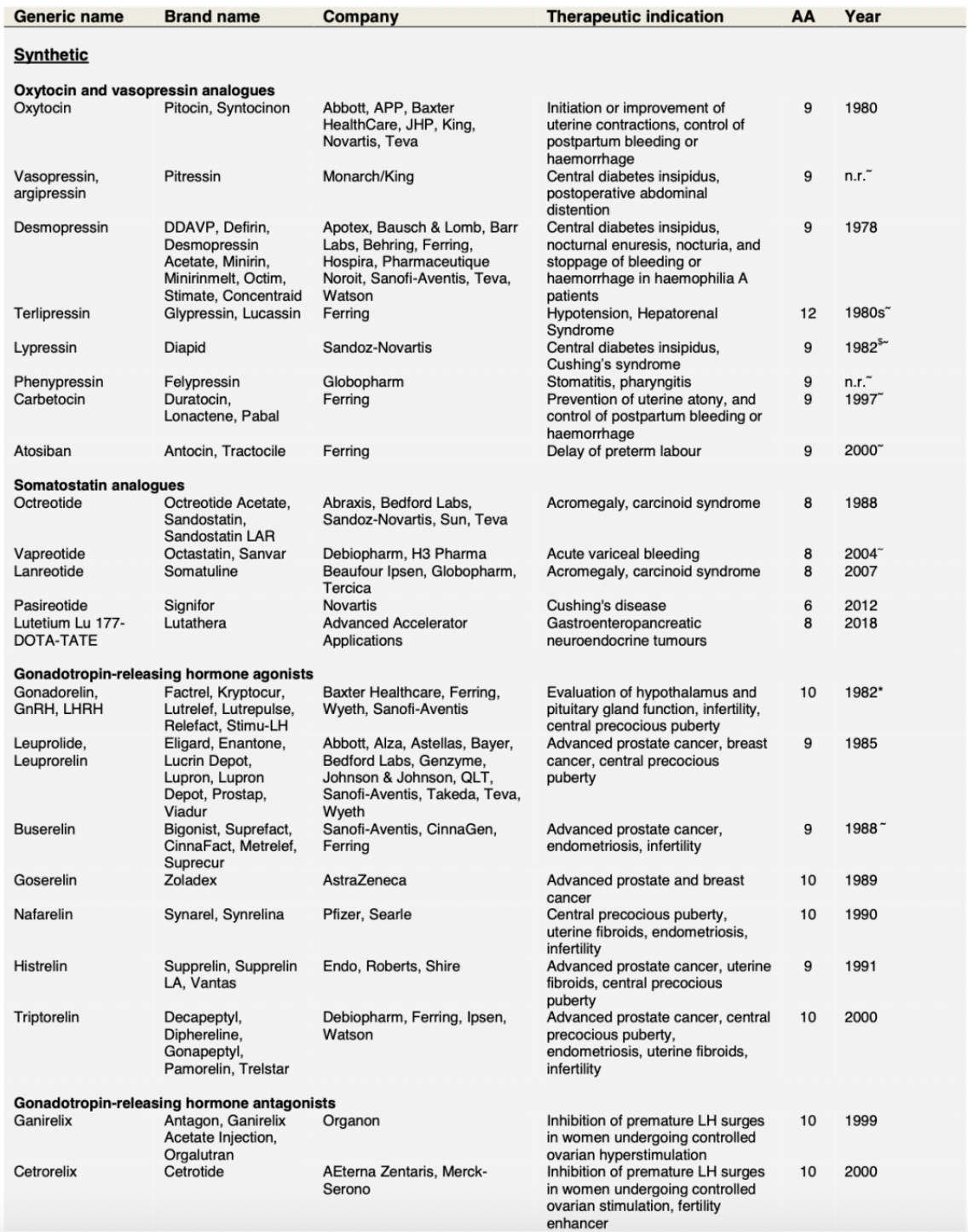
Peptide drugs approved for the market prior to 2021
Peptide drugs based on synthetic human hormones
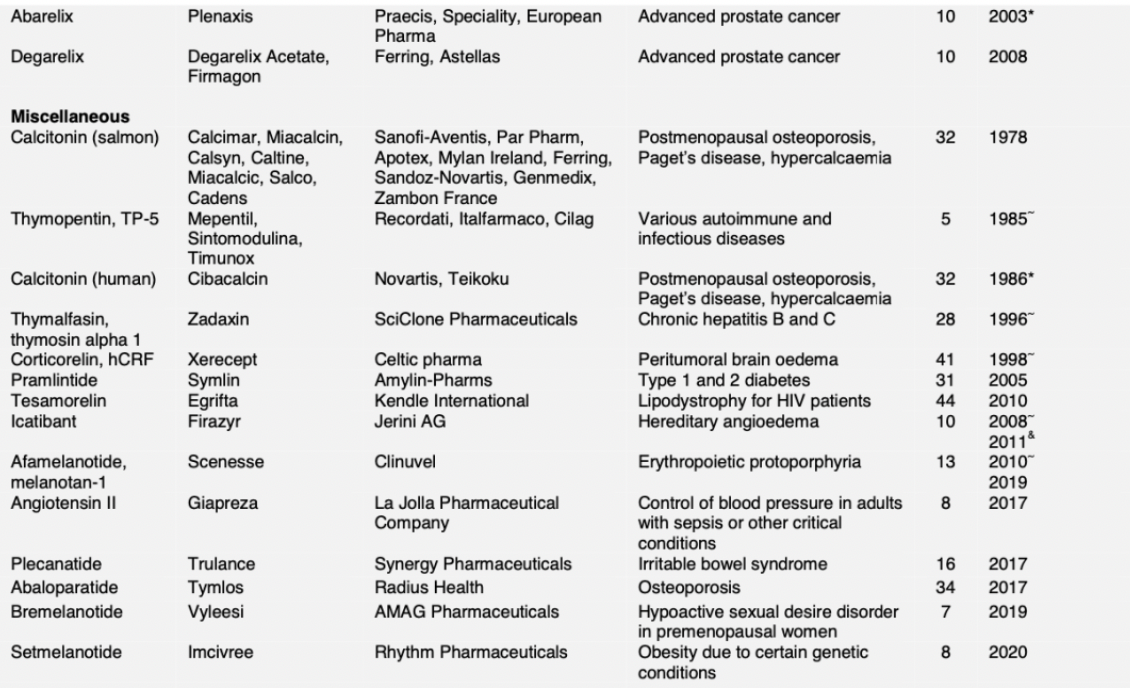
Peptide Drugs Based on Recombinant Human Hormones
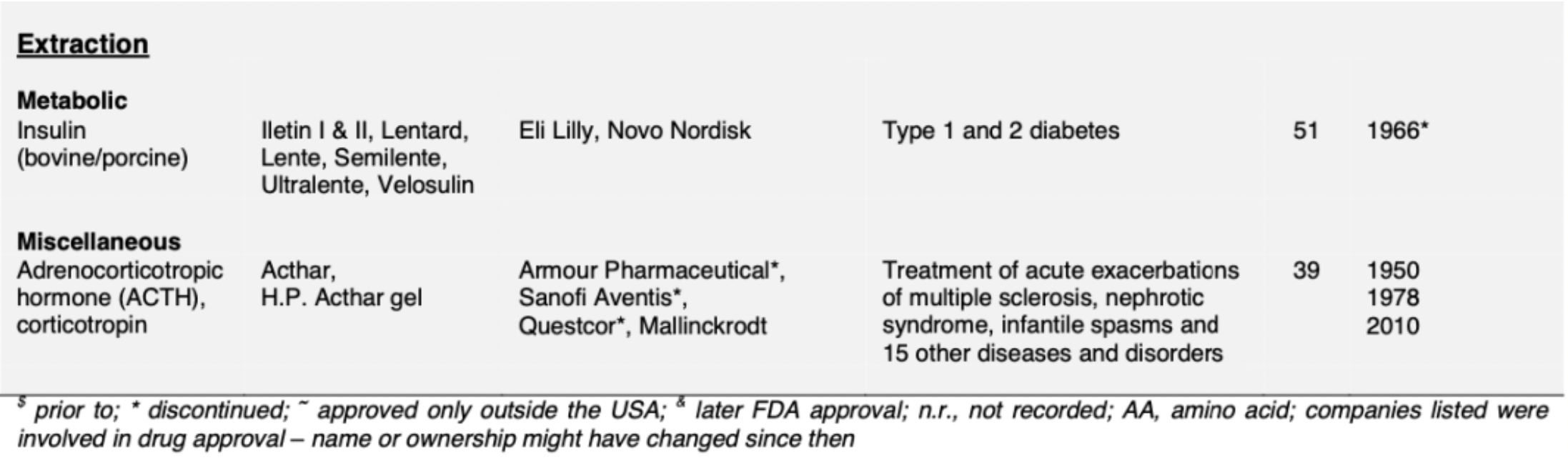
Peptide Drugs Based on Hormone Extracts
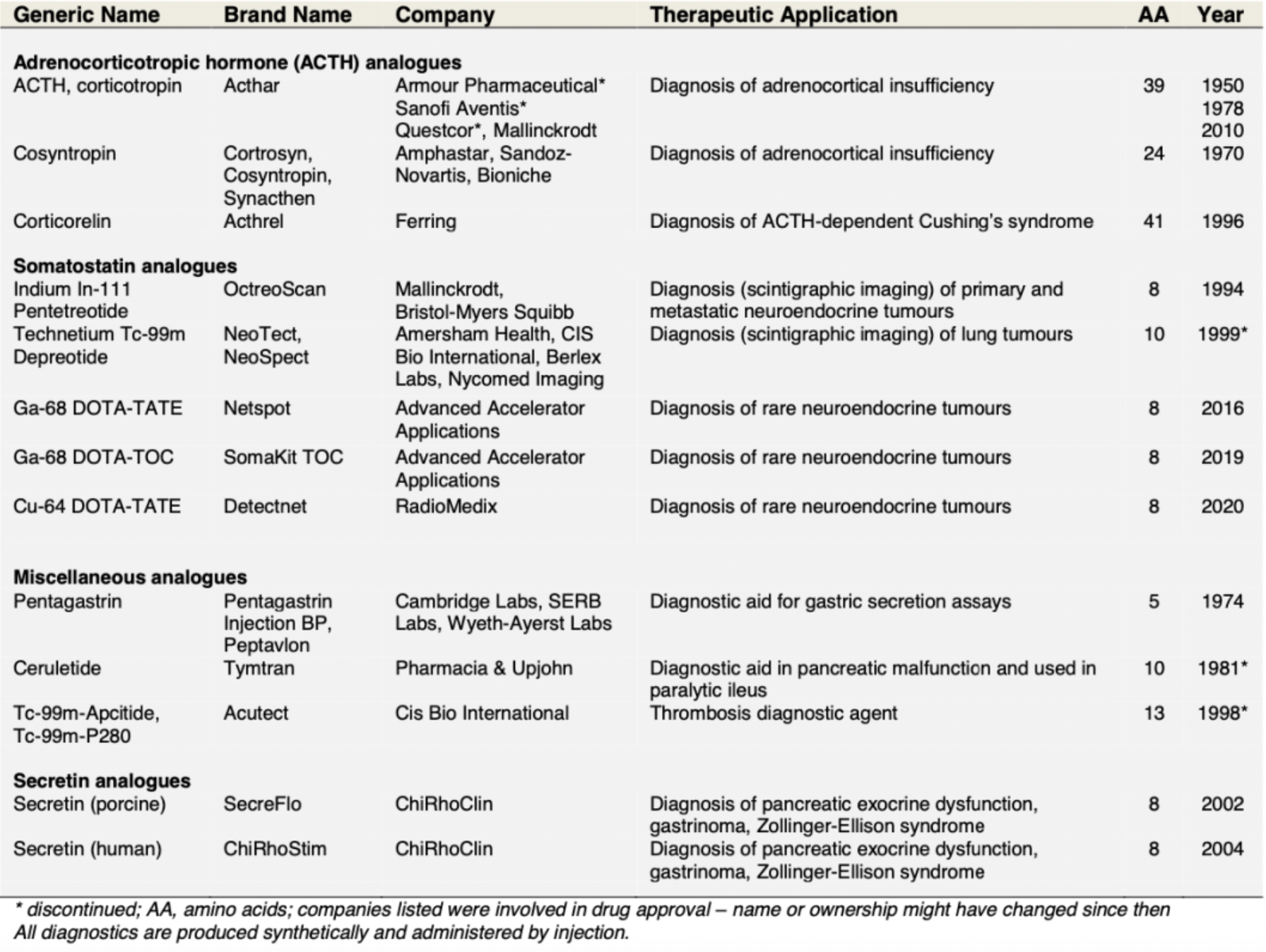
Peptide-based Diagnostic Products
Peptide drugs extracted from animals, plants, and bacteria
Peptide drugs based on serendipitous discovery and rational design
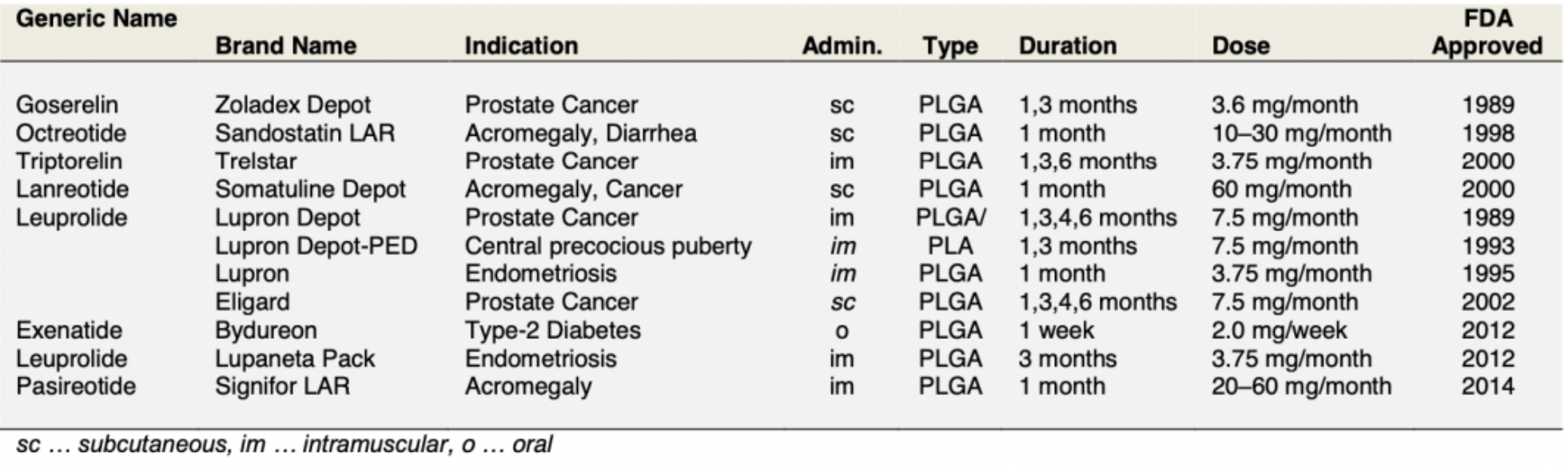
Sustained-release formulations of peptide drugs based on injectable poly(lactic-co-glycolic acid) (PLGA) or poly(lactic acid) (PLA) delivery systems
(This technology leverages biodegradable polymers such as PLGA and PLA, which form long-acting delivery carriers in the form of microparticles or microspheres by combining with peptide drugs. Since PLGA and PLA gradually degrade into non-toxic byproducts in the body and are metabolized and excreted, they are known for their excellent biocompatibility and safety as drug delivery materials.)
Representative peptide drugs
Calcitonin and Parathyroid Hormone (PTH)
Calcitonin is a peptide hormone composed of 32 amino acid residues, discovered in 1961 to effectively lower calcium ion levels in dog blood. Subsequent research has proven that calcitonin can strongly inhibit the bone resorption process. Salmon calcitonin differs from human calcitonin in sequence by 16 amino acid residues, yet its potency is 40 to 50 times higher. Salmon calcitonin was approved in 1978 for the treatment of hypercalcemia and postmenopausal osteoporosis. Initially, salmon calcitonin was a natural substance extracted from a gland analog to the thyroid gland in salmon, but a synthetic version was approved for use in 1978, and further advancements in 2005 led to the development of salmon calcitonin produced using recombinant technology.
Parathyroid hormone (PTH), which contains 84 amino acid residues, was discovered in 1925. Its action is the opposite of calcitonin's, primarily activating PTH1 and PTH2 receptors to promote the release of calcium ions from the bone's calcium stores, significantly raising the calcium content in the blood. However, prolonged elevated levels of PTH can lead to the depletion of calcium reserves in the bone, detrimental to maintaining bone health.
Due to the extremely short half-life of PTH and its analogs in the body, they are not suitable for clinical therapy. With the advancement of chemical modification techniques, researchers have adopted various strategies to extend the activity and stability of PTH analogs, such as the introduction of non-natural amino acids, N-terminal or C-terminal extensions, and disulfide bond mimetics, among others. These improvements have allowed PTH-like drugs to exert biological effects more effectively in the human body and to reduce clearance rates.
The first PTH-based therapy was Teriparatide, a recombinant fragment of the first 34 amino acid residues of human PTH, which is the biologically active portion. It was approved in 2002 for the treatment of osteoporosis. Teriparatide not only inhibits bone resorption but is also the first drug that can promote new bone formation rather than merely inhibiting the loss of old bone. This significantly improves the management of bone density and the risk of fractures.
Subsequently, with the overcoming of PTH's instability, a full-length PTH therapy was developed to control blood calcium levels in patients with hypocalcemia, which was approved in 2015. In addition, a synthetic analog similar to Parathyroid Hormone-Related Protein (PTHrP), abaloparatide, was developed. This drug shares 41% sequence homology with PTH and was approved in 2017 for the treatment of osteoporosis.
Somatostatin
Somatostatin is an endogenous hormone composed of 14 amino acid residues, which has the ability to inhibit the secretion of a variety of endocrine glands. This includes its inhibitory effects on growth hormone, insulin, gastric acid, and cholecystokinin. Due to its extremely short half-life in the body, it is not suitable for direct clinical treatment. Therefore, researchers have improved it through a series of chemical modification techniques.
Firstly, by truncating somatostatin, substituting specific amino acid residues, as well as cyclizing the N- to C-terminus, scientists have successfully enhanced the stability and biological activity of the hormone and its analogs. For instance, employing methods such as d-amino acid substitutions, incorporation of unnatural amino acids, terminal protection at the N or C end, and mimicking disulfide bonds, a series of drugs widely used in clinical practice has been developed, such as octreotide. Octreotide effectively treats conditions like acromegaly, certain types of tumors, and other related diseases, and it has a significantly prolonged duration of action in the body.
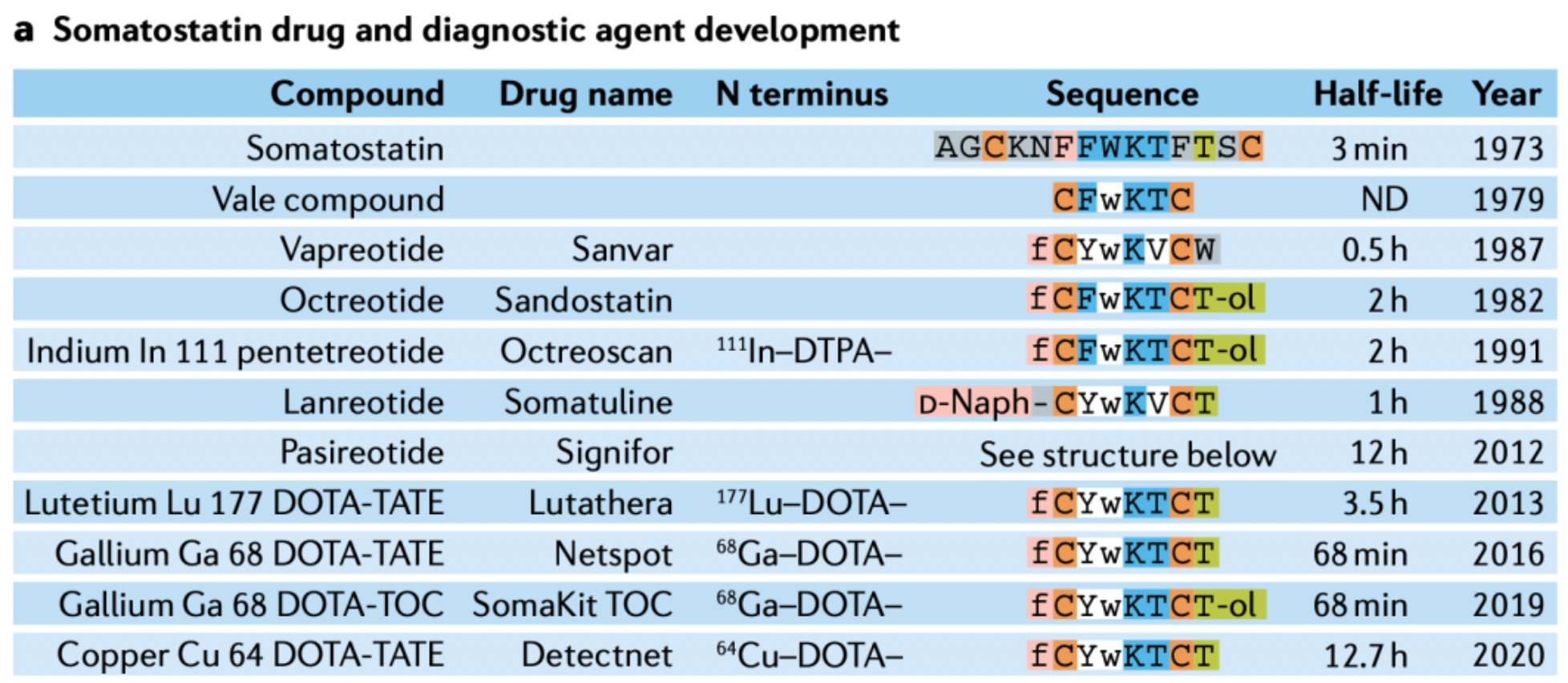
Additionally, research on somatostatin receptors has revealed that many tumor cells overexpress different subtypes of these receptors. This has not only propelled the development of subtype-selective somatostatin analogs such as lanreotide, vapreotide, and pasireotide but has also given rise to a new therapeutic field of peptide receptor radionuclide therapy (PRRT). By conjugating radioactive isotopes with somatostatin analogs, radiopharmaceuticals are formed that can be used for the diagnosis and treatment of diseases such as neuroendocrine tumors, for instance, In 111 pentetreotide, Ga 68 DOTA-TATE, and others.
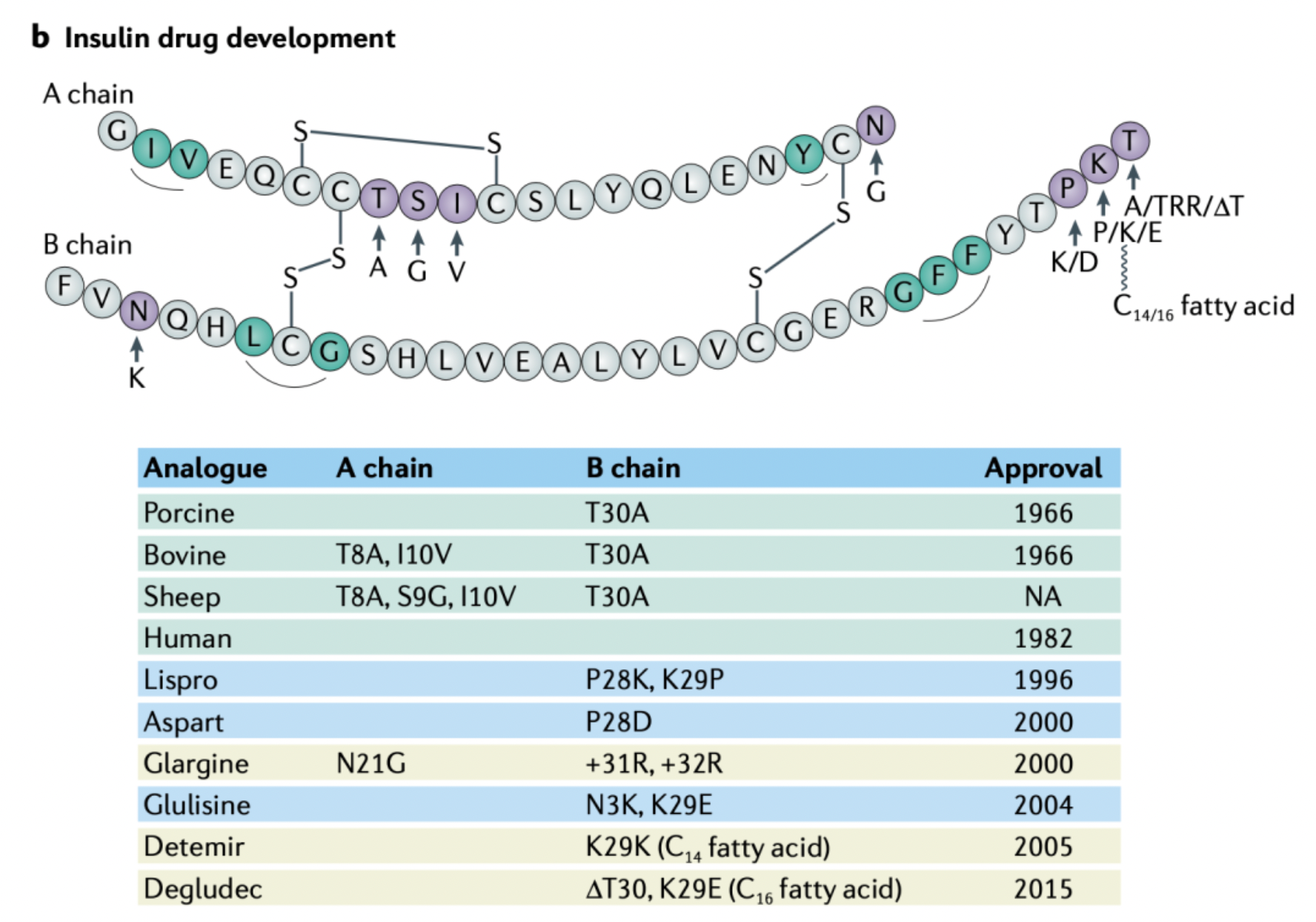
Insulin
Insulin was the first peptide drug used for the treatment of disease, first extracted from the pancreases of animals (cattle and pigs) in 1922 and applied in clinical practice. It successfully transformed the treatment approach for patients with Type 1 diabetes and remains one of the most commercially successful peptide drugs to this day, with market demand maintaining an annual compound growth rate of about 10% due to the rising incidence of obesity.
In response to the inherent limitations of insulin, such as its short metabolic half-life, researchers have employed various medicinal chemistry strategies for optimization. These include the introduction of non-natural amino acids, protection and extension at the N-terminus or C-terminus, and mimicking disulfide bond structures to enhance the stability and biological activity of insulin. These improvements not only increased the efficacy and selectivity of insulin analogs but also improved their pharmacokinetic properties. As a result, a range of insulin formulations with better therapeutic effects and more convenient usage have been developed, such as long-acting insulins and their analogs.
Moreover, with the development of recombinant DNA technology in the 1980s, insulin production entered a new phase, enabling the efficient and clean manufacturing of larger-scale peptides, overcoming the limitations of early extraction methods. By combining with lipids, large molecular proteins, and polyethylene glycol, the molecular weight of insulin molecules was further increased, effectively addressing the problem of rapid renal clearance. This extended the drug’s circulation time in plasma, thus ensuring that the medication has a more prolonged glucose-lowering effect.
Oxytocin and Vasopressin Analogs
Oxytocin is an endogenous hormone consisting of nine amino acid residues, first synthesized in its entirety by Vincent du Vigneaud's team in 1954, and is renowned for its critical role in childbirth, lactation, and social behaviors.
Oxytocin, due to its short half-life in the body (only a few minutes), has its potential as a therapeutic drug limited. To overcome this limitation, researchers have employed a range of innovative medicinal chemistry approaches for structural modification. These include, but are not limited to: the use of D-amino acids to increase stability; the introduction of non-natural amino acids to alter pharmacological properties; N-terminal or C-terminal protection and extension to slow down degradation; and the exploration of disulfide bond mimetics to enhance conformational and metabolic stability.
Through these chemical modification techniques, oxytocin analogs have been developed that possess longer duration of action, higher activity, and selectivity. For example, desmopressin is a modified vasopressin analog that has shown superior effects to natural hormones in the treatment of diabetes insipidus. Moreover, oxytocin analogs are used clinically to induce uterine contractions to facilitate childbirth and play an important role in reducing postpartum hemorrhage, treating certain gynecological disorders, and more.
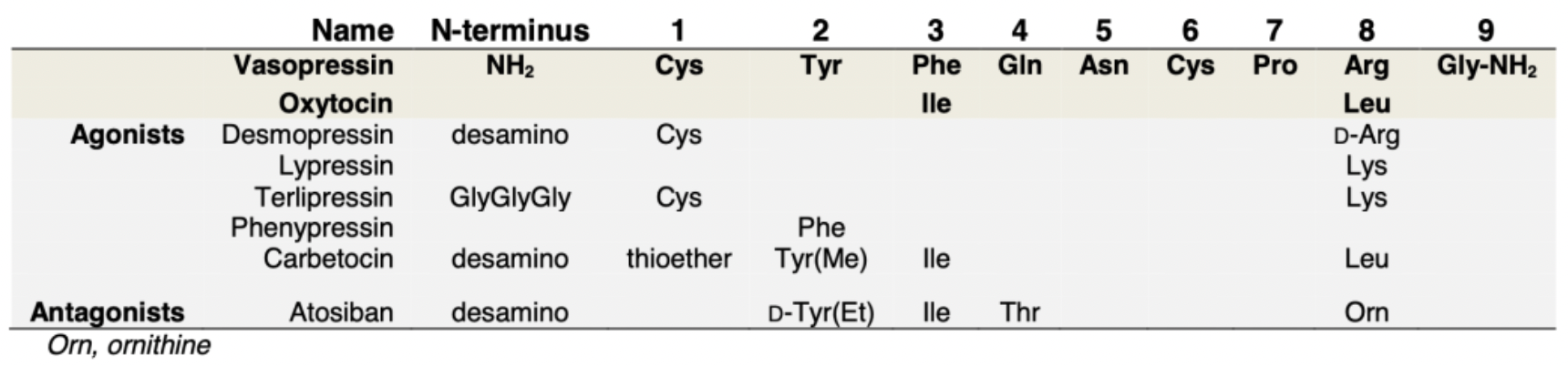
Vasopressin and Lys8-vasopressin were once used to treat central diabetes insipidus, but later were replaced by desmopressin, which has greater proteolytic stability. Desmopressin is one of the first peptide medications capable of being administered orally and via the nasal route, with a half-life of approximately 1.5 to 2.5 hours.
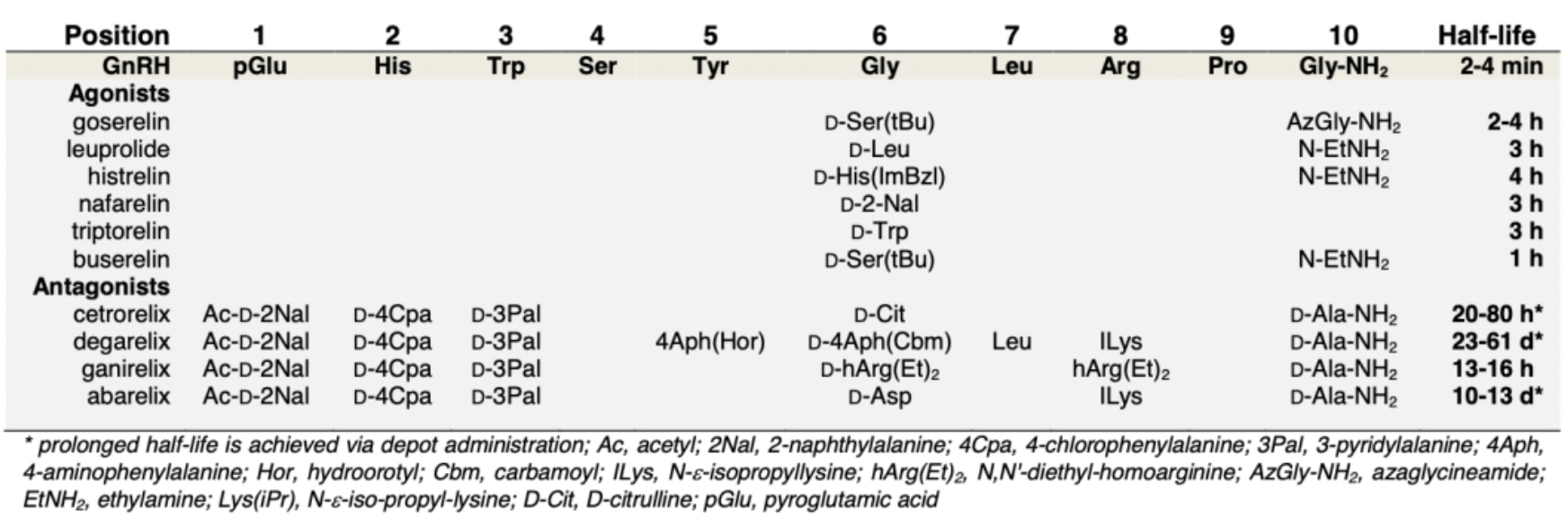
Gonadotropin-Releasing Hormone Analogs
Gonadotropin-Releasing Hormone (GnRH) analogs are synthetic drugs designed by modifying the naturally occurring GnRH, a hormone that plays a critical role in the regulation of gonadal sex hormone secretion.
In the production process of GnRH superagonists, glycine at position 6 is replaced by a different D-amino acid, which enhances the binding affinity to its receptor and imparts resistance to proteolytic enzymes. By substituting the C-terminal glycinamide with ethylamine or a bio-mimetic hydrazide glycine derivative, it not only prevents degradation by carboxypeptidase like the natural amide but also imparts increased hydrophobicity, thus increasing the potency and duration of action of the molecule.
Initial attempts at preparing antagonists involved the introduction of D-amino acids at position 6; however, histaminergic skin reactions after subcutaneous injection in rats hindered further clinical development. To avoid the risk of edema, researchers replaced D-arginine with a neutral D-urethane-alkyl-amino acid. In comparison to agonists, antagonists utilize a greater number of non-natural amino acid components, with every residue being modified in at least one antagonist except for positions 4, 7, and 9.
Amylin analogs
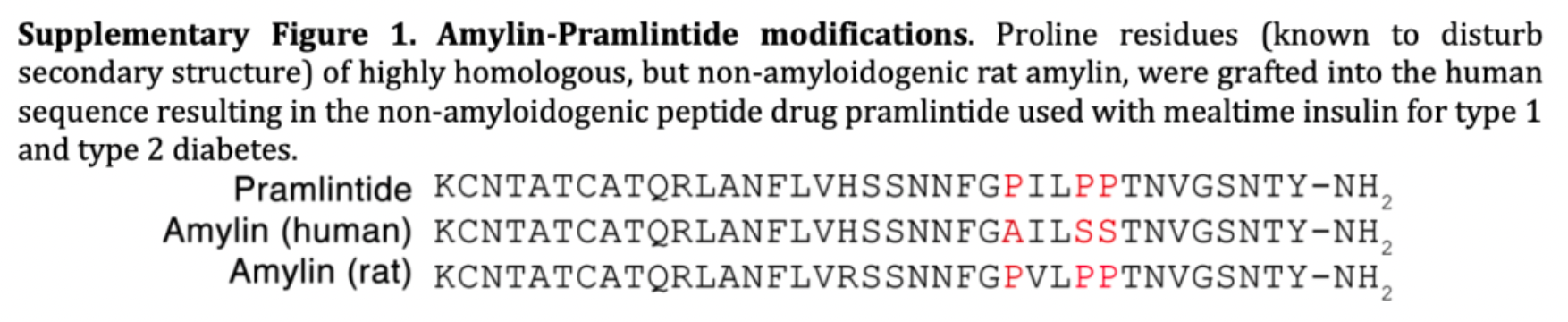
Amylin is an endocrine hormone composed of 37 amino acids that is primarily secreted by pancreatic beta cells. It plays a key role in blood glucose regulation within the body, particularly in suppressing the release of glucagon after meals and slowing down the rate of gastric emptying.
Pramlintide, composed of 31 amino acids, is a synthetic analogue of human amylin, which is a peptide hormone co-secreted with insulin from pancreatic β-cells following a meal. Patients with Type 1 diabetes exhibit abnormally low levels of insulin, while those with Type 2 diabetes have levels that are higher than normal. Due to the high propensity for amyloidogenesis in endogenous human amylin, researchers have taken inspiration from the highly homologous but non-amyloidogenic rat amylin, specifically the proline residues known to disrupt secondary structure, and incorporated them into the human amylin sequence, resulting in the development of pramlintide.
GLP-1 Peptide
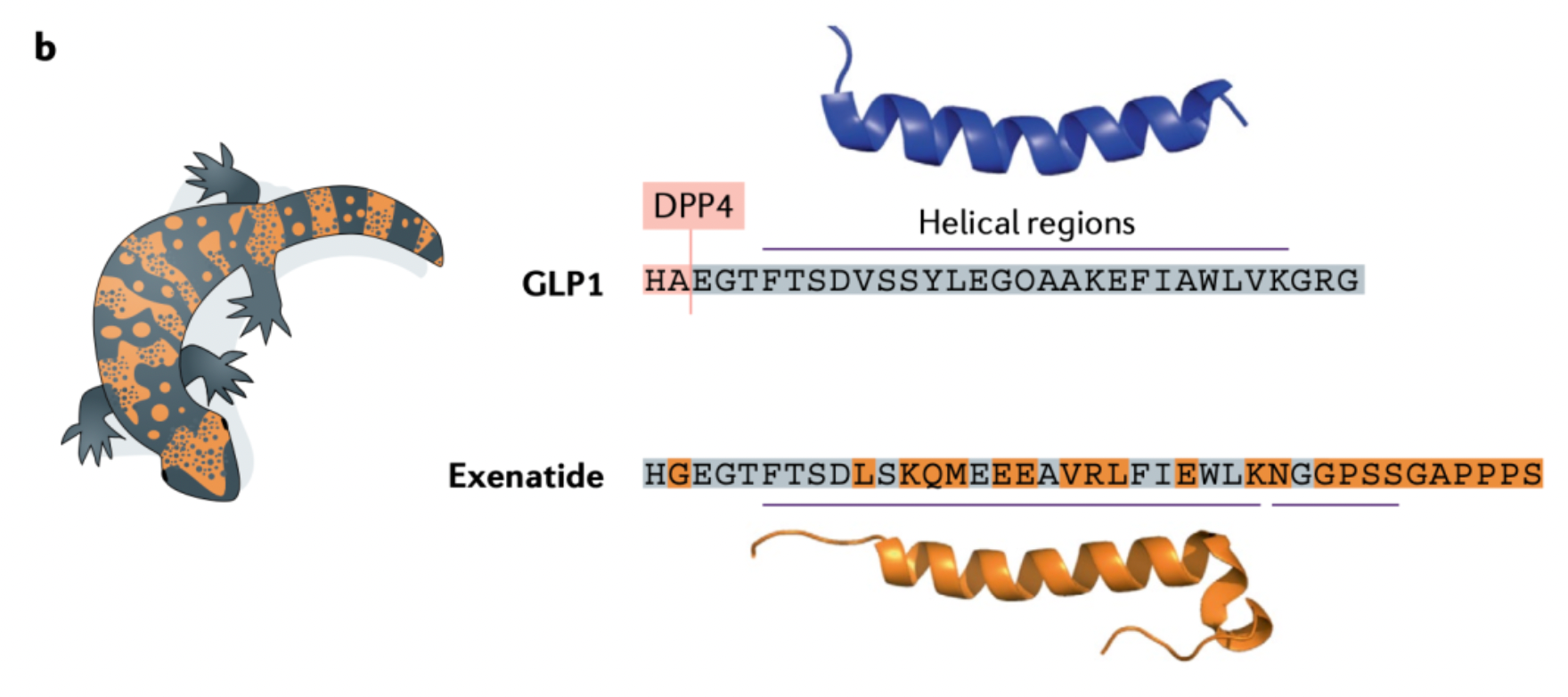
GLP-1 (Glucagon-like peptide-1) is an endogenous incretin hormone composed of 31 amino acid residues. It significantly enhances glucose-dependent insulin secretion, and is capable of inhibiting postprandial glucagon release, slowing gastric emptying, and affecting appetite. Thus, it plays a crucial role in the treatment of diabetes.
Early research found that intravenous infusion of GLP-1(7–37) has a significant impact on insulin secretion and blood glucose levels in type 2 diabetes patients, which led to substantial efforts to develop it into a therapeutic drug. However, GLP-1(7–37) is rapidly degraded by dipeptidyl peptidase-4 (DPP4) and cleared through the kidneys within 1 to 2 minutes. Although substituting other short side-chain amino acids for alanine at position 2 can protect the molecule from enzymatic degradation, the rapid renal clearance rate still renders it unsuitable for therapeutic use.
In the early 1990s, a 39-residue peptide with 53% homology to GLP-1(7–37) was isolated from the venom of the Gila monster and named "exendin-4." Studies found that exendin-4 is a full agonist for the GLP-1 receptor, stable against DPP4 degradation, and has a lower rate of renal clearance in humans (5 to 7 hours). This peptide was later developed into a drug (with the trade name exenatide, administered subcutaneously twice a day) for the treatment of type 2 diabetes.
Since then, several other GLP-1 receptor agonists, including liraglutide, albiglutide, dulaglutide, lixisenatide, and semaglutide, as well as a long-acting formulation of exenatide, have subsequently been approved for the treatment of type 2 diabetes or obesity.
The text also mentions peptide drug discovery strategies, including venomomics and display technologies. The former utilizes bioinformatics to analyze the genomes and transcriptomes of venomous creatures such as venomous snakes, combined with proteomic data obtained from raw venom samples, to identify a large number of potential therapeutic toxin peptides. The latter involves constructing large-scale peptide libraries and screening for high-affinity ligands against specific targets. For example, the cyclic peptide zilucoplan, derived from Ra Pharmaceuticals' mRNA display platform, has entered phase III clinical trials for the treatment of generalized myasthenia gravis.
In terms of medicinal chemistry strategies, researchers are focused on improving the metabolic stability and plasma half-life of peptide drugs by employing techniques such as N-terminal acetylation, N-methylation, the use of D-amino acids or non-natural amino acids, and amide bond analogs (such as thioamides, peptide mimetics, and β-amino acids). Additionally, cyclization from N to C termini and disulfide bond mimetics (specifically thioether bonds) are increasingly being applied in peptide drug design to modify their metabolic stability and bioavailability. Simultaneously, highly stable cyclic structural frameworks such as cyclic thioethers and sunflower trypsin inhibitor analogs can serve as carriers to embed pharmacophores of therapeutic significance into their rings, thereby developing more stable and targeted oral peptide drugs, such as the marketed linaclotide and plecanatide for the treatment of constipation-predominant irritable bowel syndrome.
In the Future Outlook section, the author mentions that the trend in development of peptide drugs is expected to accelerate due to the success of biologics in breaking the traditional notion that drugs must be administered orally. The field of peptide therapeutics has matured and is capable of reliable and rapid scale-up production of structurally complex peptides of up to approximately 100 amino acids, as well as conducting effective structure-activity relationship (SAR) studies and lead compound optimization. Emerging peptide drug discovery technologies can efficiently generate potent candidate compounds with high selectivity and activity in a short amount of time. With the integration of novel delivery technologies and innovative chemical strategies, the field of peptide therapeutics is set to continue its robust growth.
Lastly, the author notes that, in particular, antimicrobial, antiviral, and anti-aging peptides have considerable potential for growth in the future. In the cosmetics industry, peptides are gaining increasing attention, as evidenced by market-available products like Argireline, a hexapeptide that acts as a botulinum toxin analogue to reduce wrinkles, the pentapeptide Palmitoyl Pentapeptide-4 (Matrixyl) which helps to mitigate wrinkles by stimulating extracellular matrix renewal in fibroblasts, and GHK-Cu, a natural tripeptide with high copper ion affinity that possesses anti-inflammatory properties and promotes the synthesis of collagen and glycosaminoglycans in skin fibroblasts.
Overall, the steady approval of peptide drugs over the past 60 years has witnessed the growth of this niche, and with advances in new drug discovery and delivery technologies, peptide therapeutics are expected to continue to hold a unique position in the pharmaceutical market, becoming a strong competitor situated between small molecule drugs and larger biological agents.