Latest Advances and Applications of Bispecific Antibodies in Cancer Treatment
On March 6th, the journal Nature Reviews Drug Discovery published a review article discussing the latest advances and applications of bispecific antibodies (bsAbs) in cancer treatment.

Bispecific antibodies (bsAbs) offer a unique advantage due to their ability to target two different antigens simultaneously, which helps to enhance the immune system's recognition and killing of tumor cells. As of the end of 2023, 14 bsAbs have been approved: 11 for cancer treatment and 3 for non-oncological indications. BsAbs come in various structural formats, target different antigens, and mediate antitumor functions through different molecular mechanisms.
In the study, the authors outlined recent advances in the application of bsAbs in the field of cancer therapy, focusing on bsAbs that are either approved or in clinical development stage. This includes but is not limited to: bispecific antibody-mediated dual signaling pathway modulators, tumor-targeted receptor agonists, bsAb-drug conjugates, bispecific T cells, natural killer cells, and innate immune cell activators, as well as bispecific checkpoint inhibitors and co-stimulators.
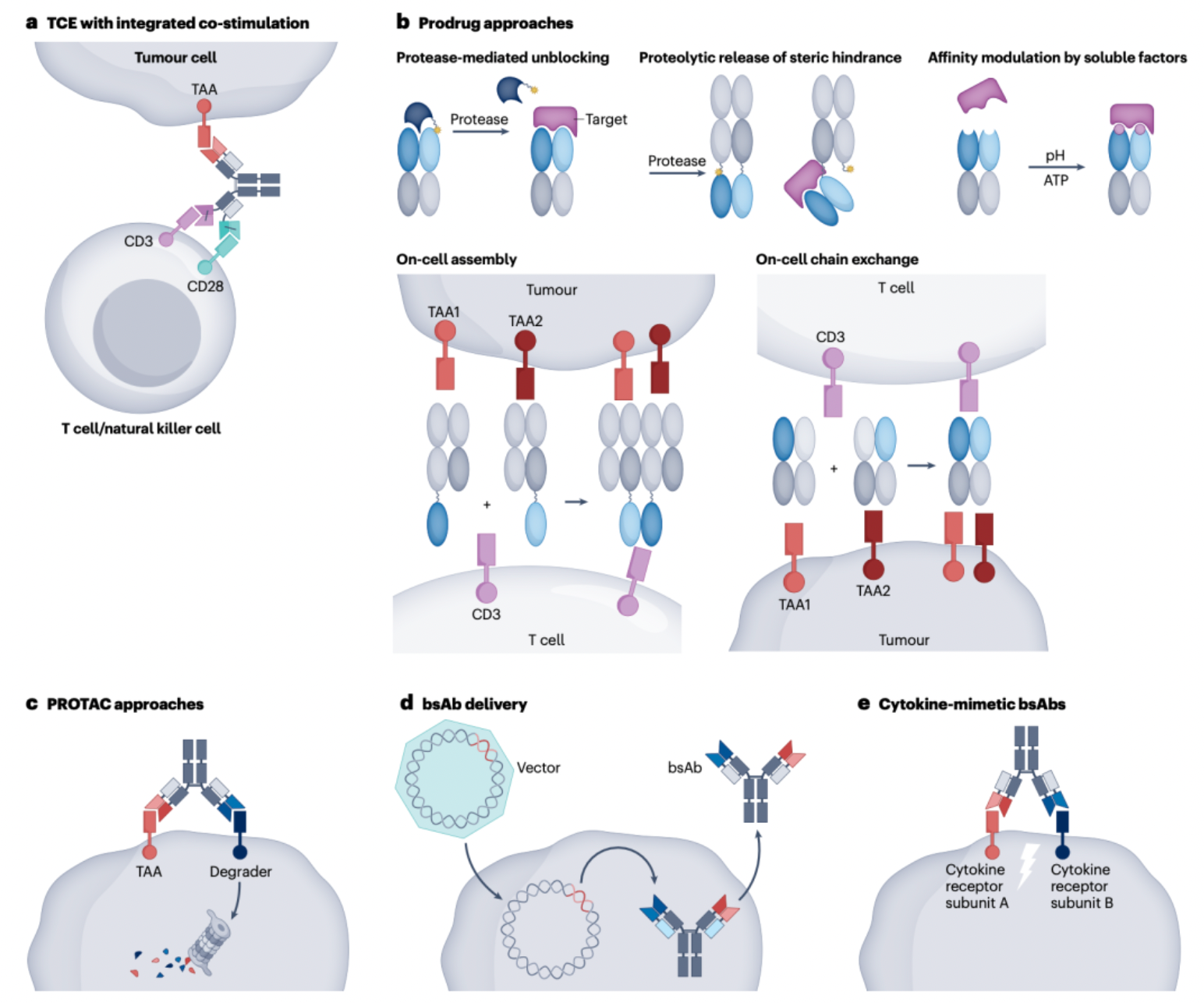
Furthermore, the authors also envisioned next-generation bsAbs that are in early development stages, which include trispecific antibodies, bsAb prodrugs, bsAbs that induce tumor-target degradation, and bsAbs that mimic cytokine functions. These novel bsAbs hold the promise to further expand the range and strategies of cancer treatment, providing more precise and efficient therapeutic options.
Current Status of Bispecific Antibody Research
Over the past decade, bispecific antibodies (bsAbs) have garnered significant attention due to their unique multimodal mechanisms of action. Between 2021 and 2023, nine bsAbs have been approved for cancer treatment, reflecting the development trajectory of such antibodies as novel therapeutic agents. The success of bsAbs lies in their ability to surpass the therapeutic effects of natural monospecific antibodies, for instance by recruiting immune effector cells to cancer cells, or by targeting different signaling pathways simultaneously with one molecule.
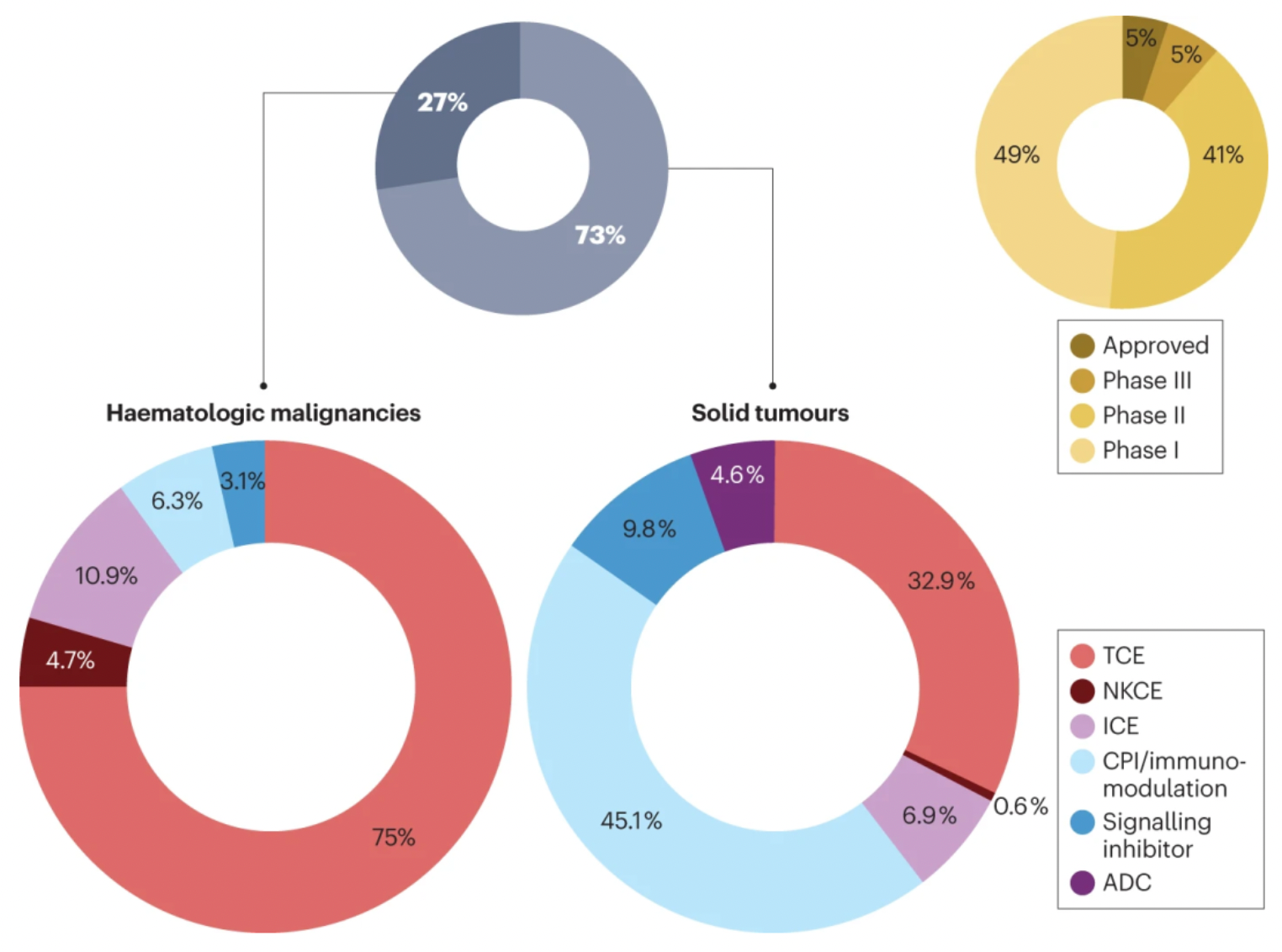
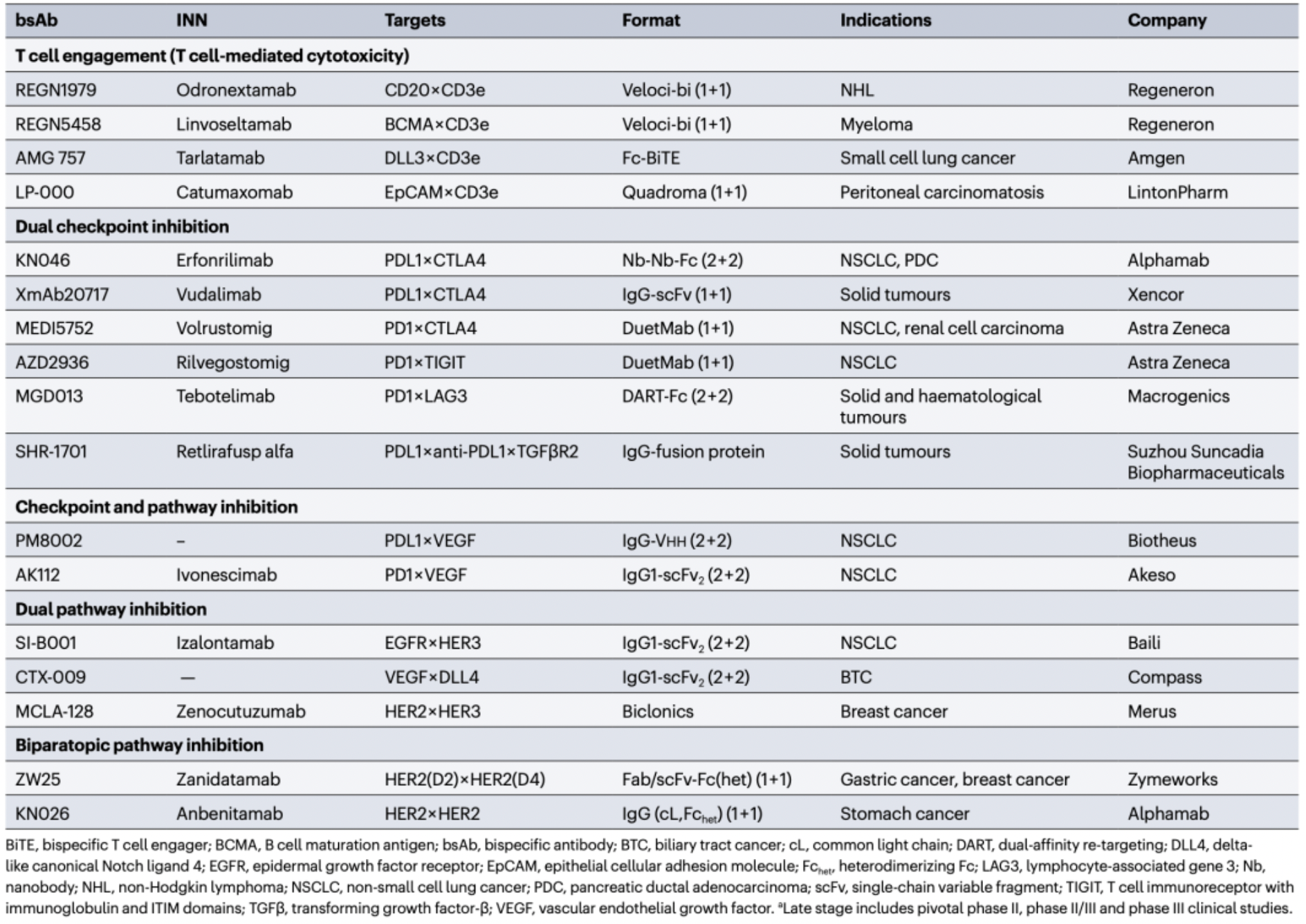
According to statistics, there are currently over 200 bsAbs in clinical development. Among these, 50% have entered Phase II or Phase III clinical trials, and some have already been approved for marketing. Approximately three-quarters of bsAbs are being developed for the treatment of solid tumors, and within the realm of solid tumor therapy, T cell engagers (TCEs, accounting for 32.9%) as well as bsAbs with checkpoint inhibition and/or immunomodulatory mechanisms (accounting for 45.1%) hold a dominant position.
In contrast, bsAbs targeting hematological malignancies are primarily composed of TCEs (accounting for 75%) and other mechanisms of immune activation (accounting for 21.9%). These mechanisms usually achieve checkpoint inhibition and/or immunomodulatory effects on natural killer cells and other immune cells through the exploitation of highly tumor-selective or lineage-specific antigens. Notably, around 10% of bsAbs for the treatment of solid tumors have adopted a dual signal inhibition strategy.
Below is an overview of the 11 bispecific antibodies approved for cancer treatment:
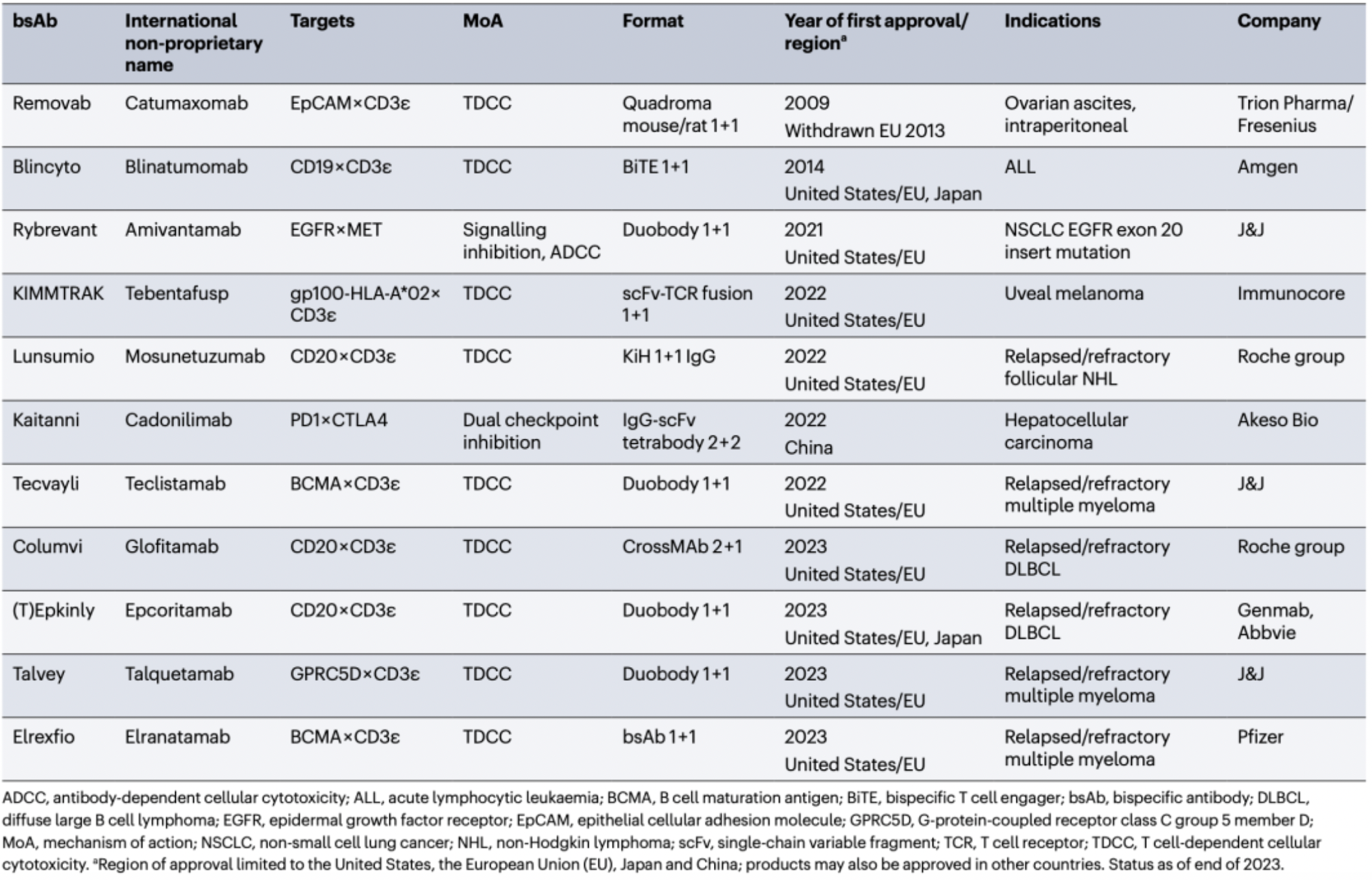
Catumaxomab (Removab): The first approved bispecific antibody (bsAb), developed in collaboration by Trion Pharma and Fresenius, targets EpCAM and CD3ε, and was used for the treatment of malignant ascites (such as that associated with ovarian cancer), but was withdrawn from the EU market in 2013.
Blinatumomab (Blincyto): Developed by Amgen, this bispecific T cell engager (TCE) targets CD19 and CD3ε with a BiTE 1+1 format. It was approved in 2014 in the United States, European Union, and Japan for the treatment of acute lymphoblastic leukemia (ALL).
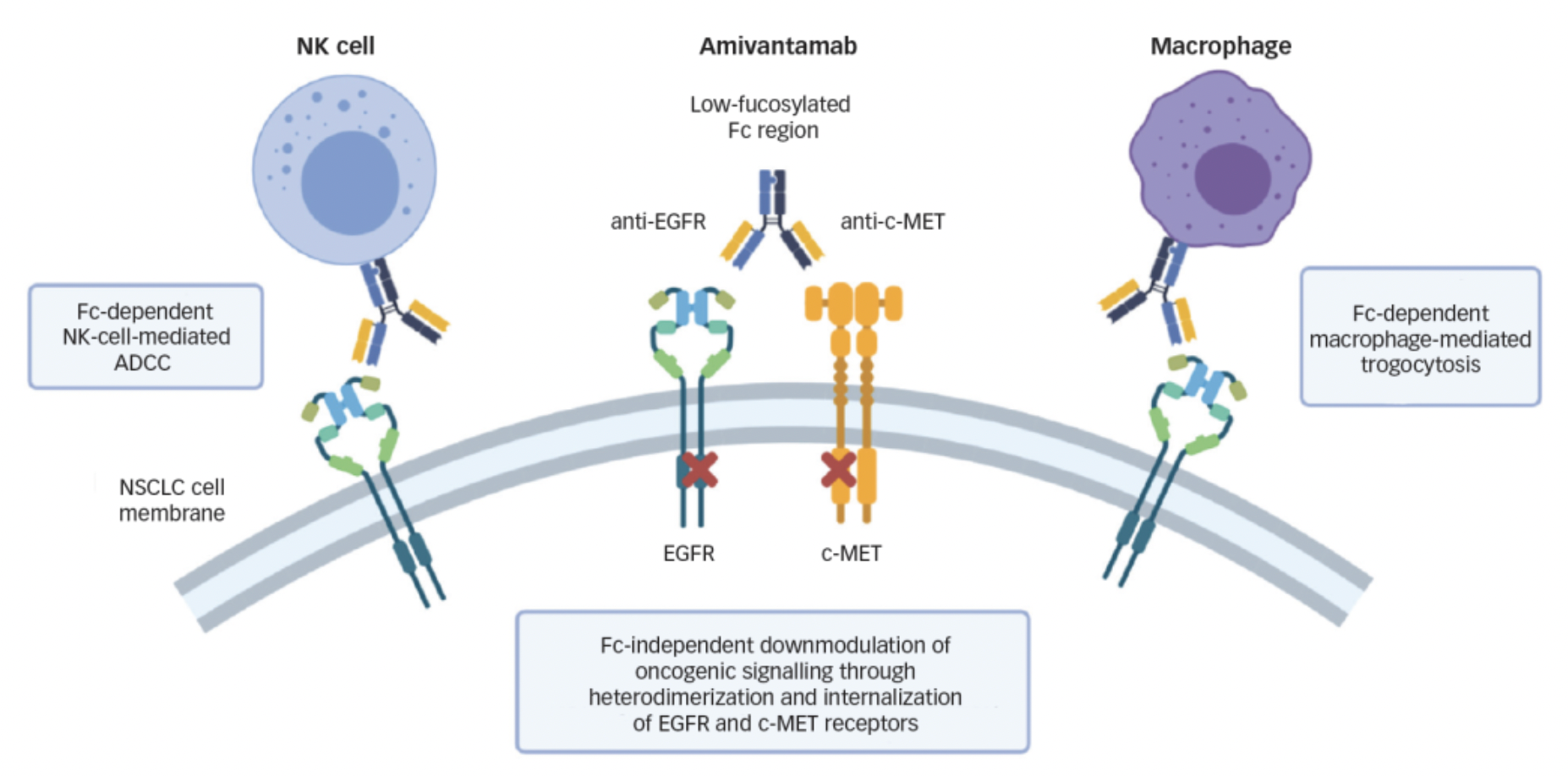
Amivantamab (Rybrevant): Developed by J&J, this agent targets both EGFR and MET. Its mechanism of action includes signal transduction inhibition and antibody-dependent cellular cytotoxicity (ADCC) effects, using a Duobody 1+1 format. It was approved in the United States and European Union in 2021 for the treatment of non-small cell lung cancer (NSCLC) with EGFR exon 20 insertion mutations.
Tebentafusp (KIMMTRAK): Produced by Immunocore, this agent targets the gp100-HLA-A*02 complex and CD3ε. It is a TCE in the form of an scFv-TCR fusion protein. It was approved in 2022 in the United States and European Union for the treatment of uveal melanoma.
Mosunetuzumab (Lunsumio): Developed by Roche, this is a bispecific TCE that targets CD20 and CD3ε, using a KiH 1+1 IgG format. It was approved in 2022 in the United States and European Union for the treatment of relapsed/refractory follicular lymphoma.
Cadonilimab (Kaitanni): Developed by Akeso, a Chinese biopharmaceutical company, this agent targets PD1 and CTLA4 and is classified as a dual immune checkpoint inhibitor. It has an IgG-scFv tetrabody 2+2 structure and was approved in China in 2022 for the treatment of hepatocellular carcinoma.
Teclistamab: Also introduced by J&J, teclistamab is a bispecific T-cell engager (TCE) targeting BCMA and CD3ε. Utilizing a Duobody 1+1 structure, it was approved in 2022 in the United States and the European Union for the treatment of relapsed/refractory multiple myeloma.
Glofitamab (Columvi): Originating from the Roche Group, glofitamab is a CD20 and CD3ε bispecific TCE using a CrossMAb 2+1 structure. It received approval in 2023 in the United States and the European Union for the treatment of relapsed/refractory diffuse large B-cell lymphoma (DLBCL).
Epcoritamab (T)Epkinly: Jointly developed by Genmab and AbbVie, epcoritamab is also a TCE targeting CD20 and CD3ε. It features a Duobody 1+1 structure and was approved in 2023 in the United States, the European Union, and Japan for the treatment of relapsed/refractory DLBCL.
Talquetamab: Another product from J&J, talquetamab targets GPRC5D and CD3ε, and is also a TCE type. Using a Duobody 1+11 structure, it was approved in 2023 in the United States and the European Union for the treatment of relapsed/refractory multiple myeloma.
Elranatamab (Elrexfio): Developed by Pfizer, elranatamab targets BCMA and CD3ε as a TCE. With a bsAb (bispecific antibody) 1+1 structure, it was approved in 2023 in the United States and the European Union for the treatment of relapsed/refractory multiple myeloma.
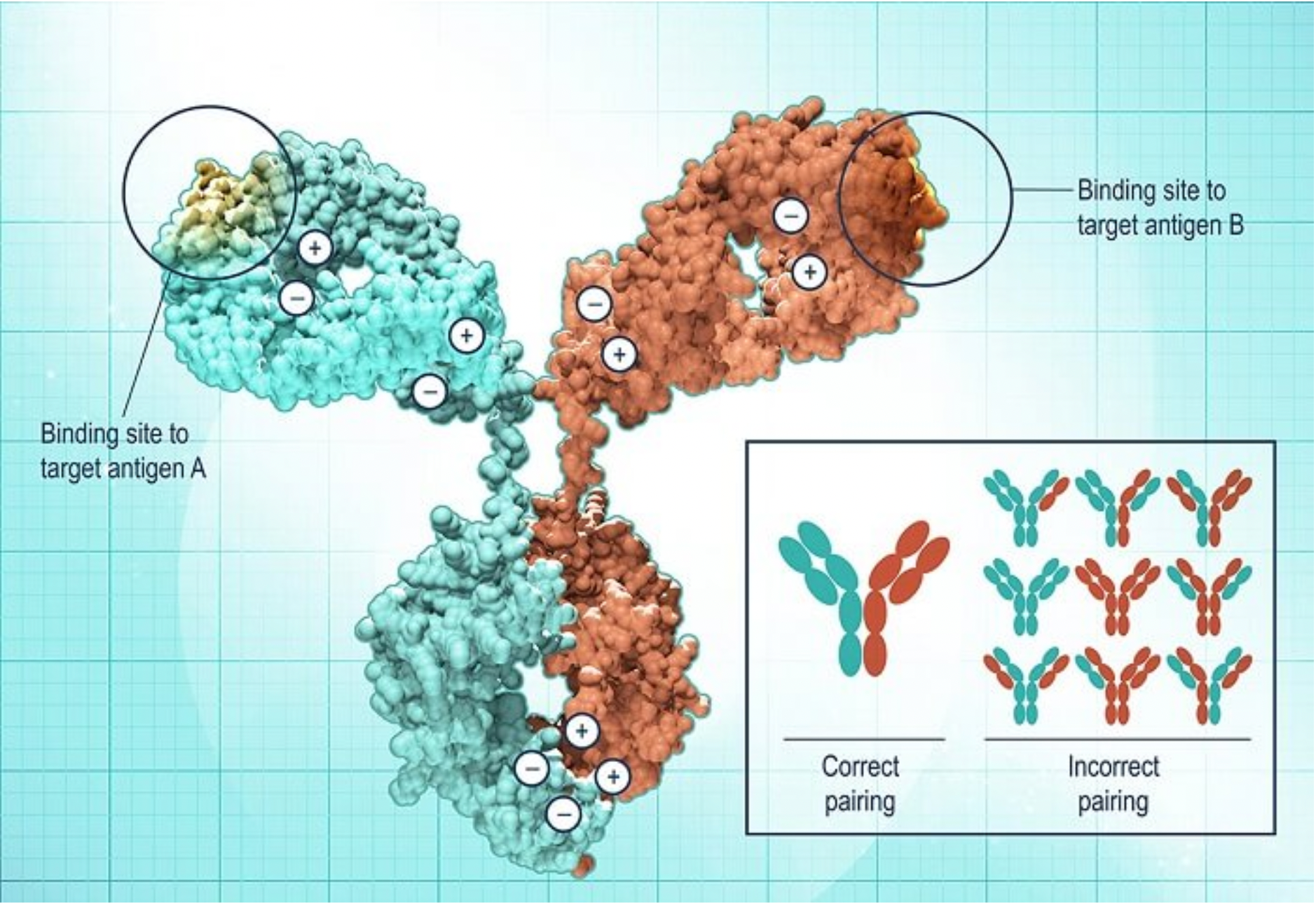
The discovery of new bsAbs is primarily driven by the underlying biological principles, and it is necessary to match them with optimal bsAb designs in order to select the correct structural forms, affinity ranges, and epitopes. Characteristics such as target selection, epitope positioning, affinity, valency, distance between binding sites, molecular size, flexibility, and the presence of an Fc region and its mediated effector functions have profound impacts on the functional attributes and developmental feasibility.
Based on whether they engage T-cells, the marketed bsAbs can be categorized into T-cell engaging and non-T-cell engaging types.
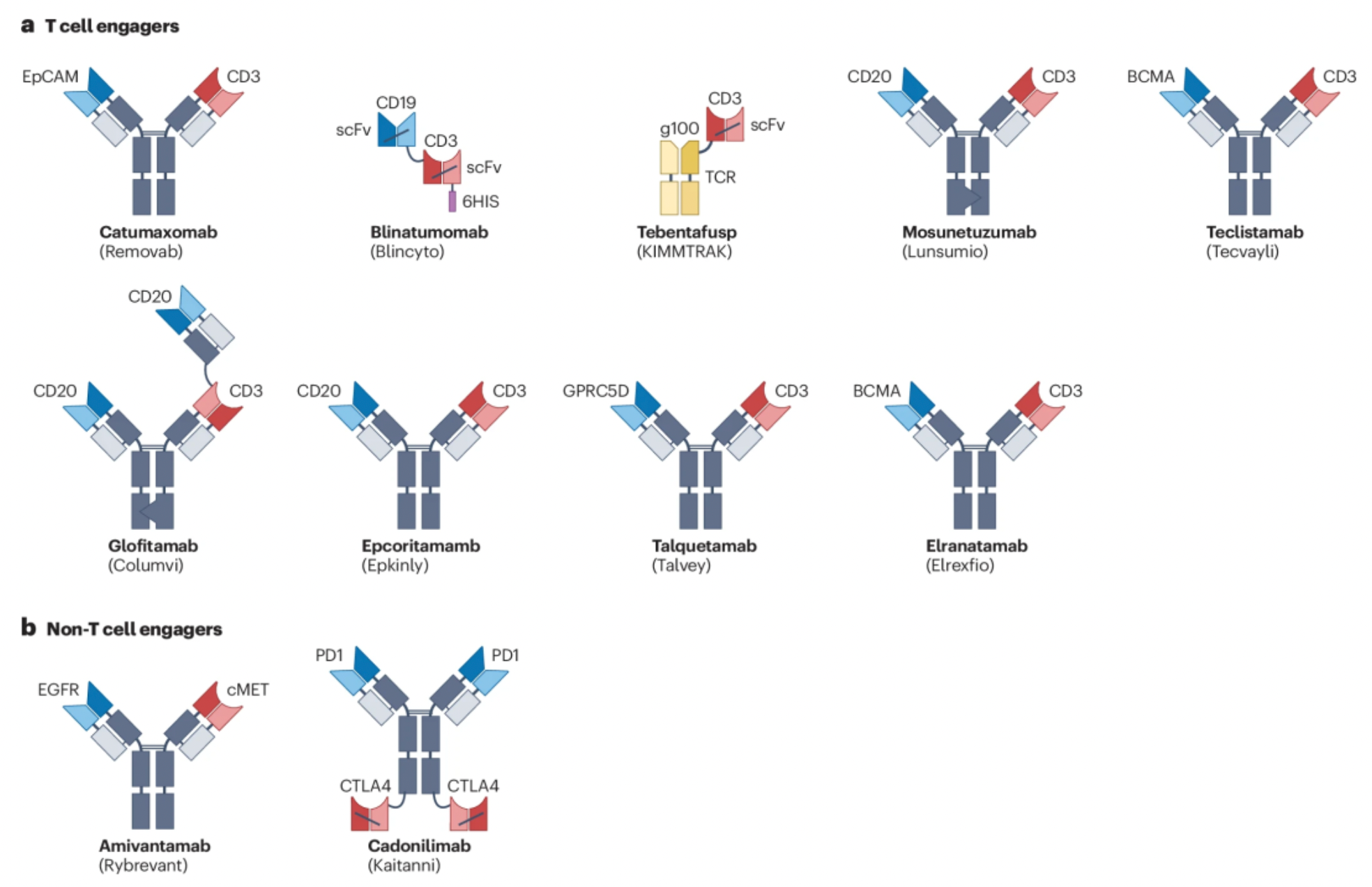
T cell engager (TCE) category of bsAbs: The primary purpose of designing this class of antibodies is to connect T cells and tumor cells via specific antigen-binding sites, thereby activating the cytotoxic activity of T cells against tumor cells. Among the 11 approved bsAbs, 6 have structures similar to IgG, consisting of two heavy chains (with the constant region depicted in dark grey, VH domains in dark blue or dark red) and two light chains (constant region in light grey, VL domains in light blue or light red). Most of these bsAbs adopt a 1+1 ratio, meaning each antigen has one binding site; additionally, there is one TCE that utilizes a 2+1 ratio model by fusing an extra Fab fragment onto one heavy chain, allowing it to bind two different antigens simultaneously.
Non-T cell engager category of bispecific antibodies: These bsAbs include different types of constructions. For example, blinatumomab is an Fc-fragment lacking fusion protein composed of two single-chain variable fragments (scFv) stitched together; tebentafusp is a product where an scFv fragment is fused with a T cell receptor (TCR) fragment. There are also IgG-scFv fusion proteins with a 2+2 ratio mode, meaning they contain two full IgG domains and two scFv domains, capable of binding simultaneously to two different antigens.
Representative monoclonal antibodies in clinical research:
The mechanism of action of bsAbs
Bispecific antibodies (bsAbs) exhibit immense potential in cancer therapy due to their unique design and diverse mechanisms of action.
The following is a brief overview of the different mechanisms of bispecific antibodies and their underlying principles:
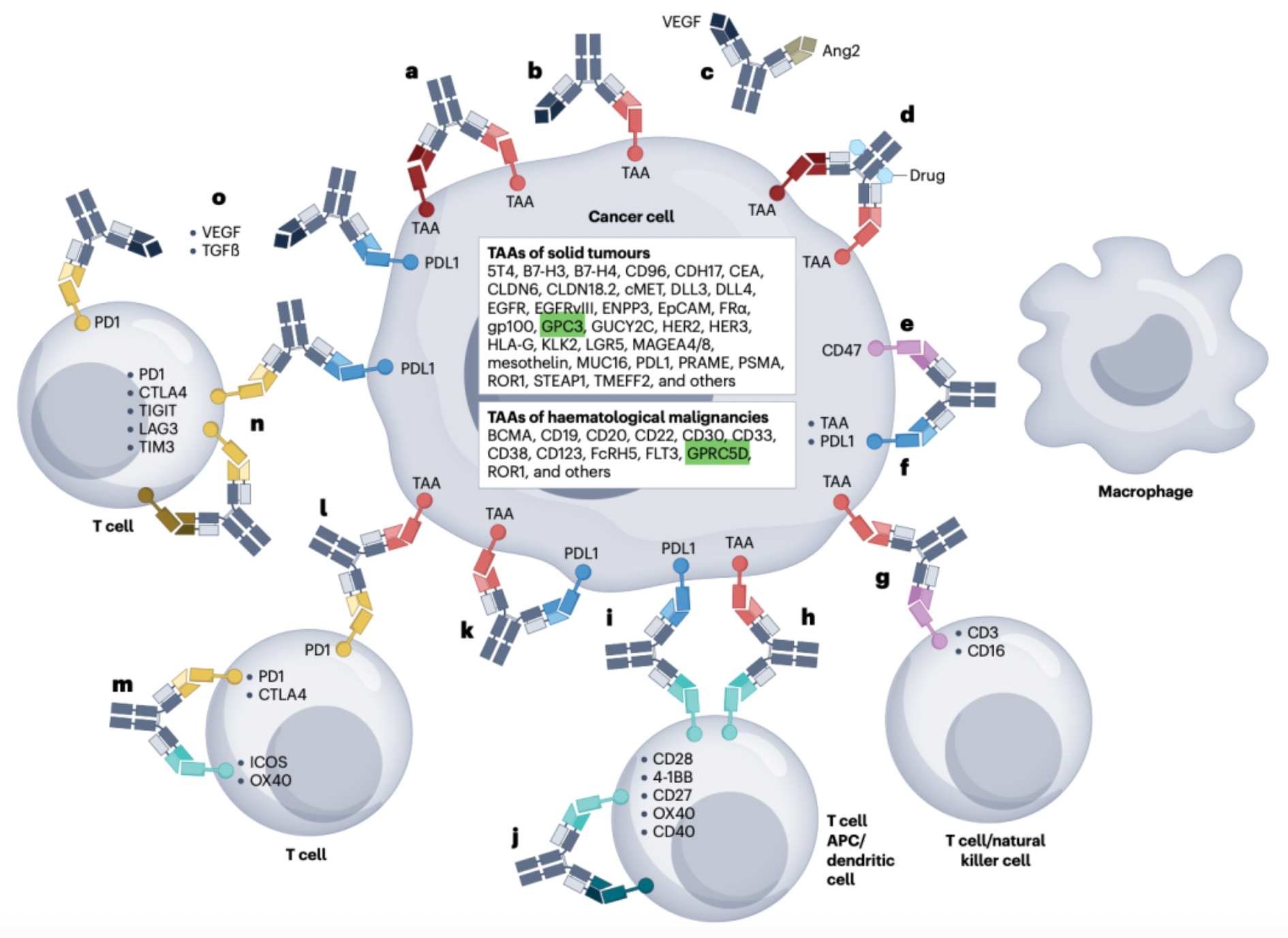
Dual receptor inhibitor bispecific antibodies: Bispecific antibodies with dual receptor-blocking capabilities can simultaneously target two different cell surface receptors, such as EGFR, HER2, and VEGF.
For instance, Amivantamab (JNJ-61186372) is a bispecific antibody designed to concurrently bind to the epidermal growth factor receptor (EGFR) and the hepatocyte growth factor receptor (MET). These receptors play key roles in the pathogenesis of non-small cell lung cancer (NSCLC), promoting the proliferation and survival of tumor cells. Traditional monospecific therapies may lead to resistance as tumor cells exploit alternative compensatory signaling pathways. However, as the first approved bispecific antibody targeting both receptor tyrosine kinases, Amivantamab can more effectively inhibit the progression of NSCLC. By simultaneously blocking both the EGFR and MET signaling pathways, it can reduce or overcome resistance due to redundancy associated with single-drug treatments.
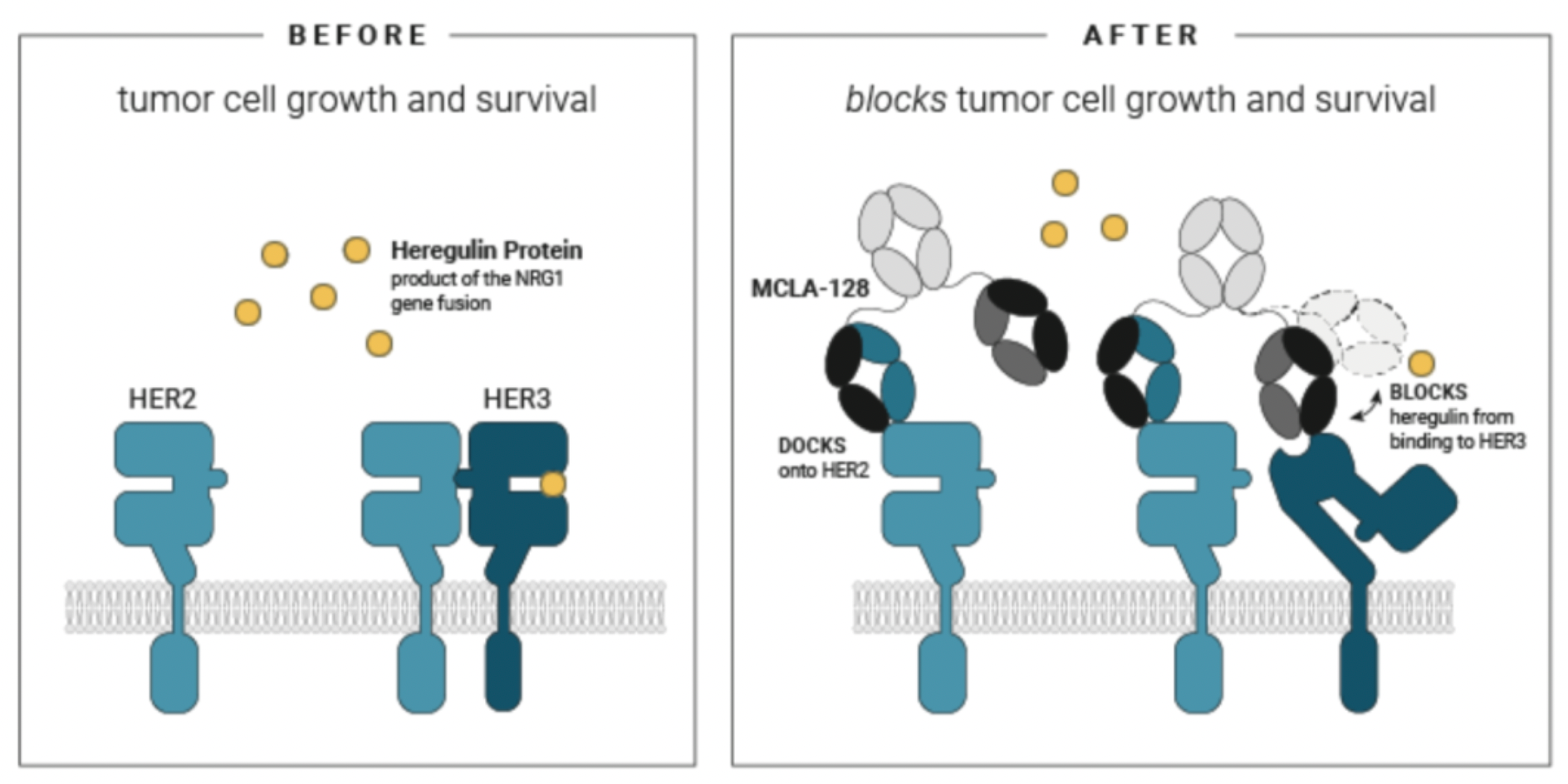
The design purpose of zenocutuzumab (MCLA-128) is to simultaneously bind to both the HER2 and HER3 receptors. This dual-targeting strategy utilizes the biological characteristic of the interactions between members of the HER family: HER2 and HER3 are capable not only of forming homodimers but can also create heterodimers with other HER family members (including EGFR), activating downstream signaling pathways that promote tumor cell growth, survival, and metastasis. In clinical studies, zenocutuzumab has been found to have therapeutic potential in patients with solid tumors harboring NRG1 gene fusions. NRG1 is a ligand for HER3, and its binding to HER3 induces the formation of the HER2/HER3 heterodimer complex, thereby driving cancer cell proliferation. By simultaneously blocking HER2 and HER3, zenocutuzumab is anticipated to prevent the activation of this pro-tumorigenic signaling pathway, thereby inhibiting the progression of this specific type of tumor.
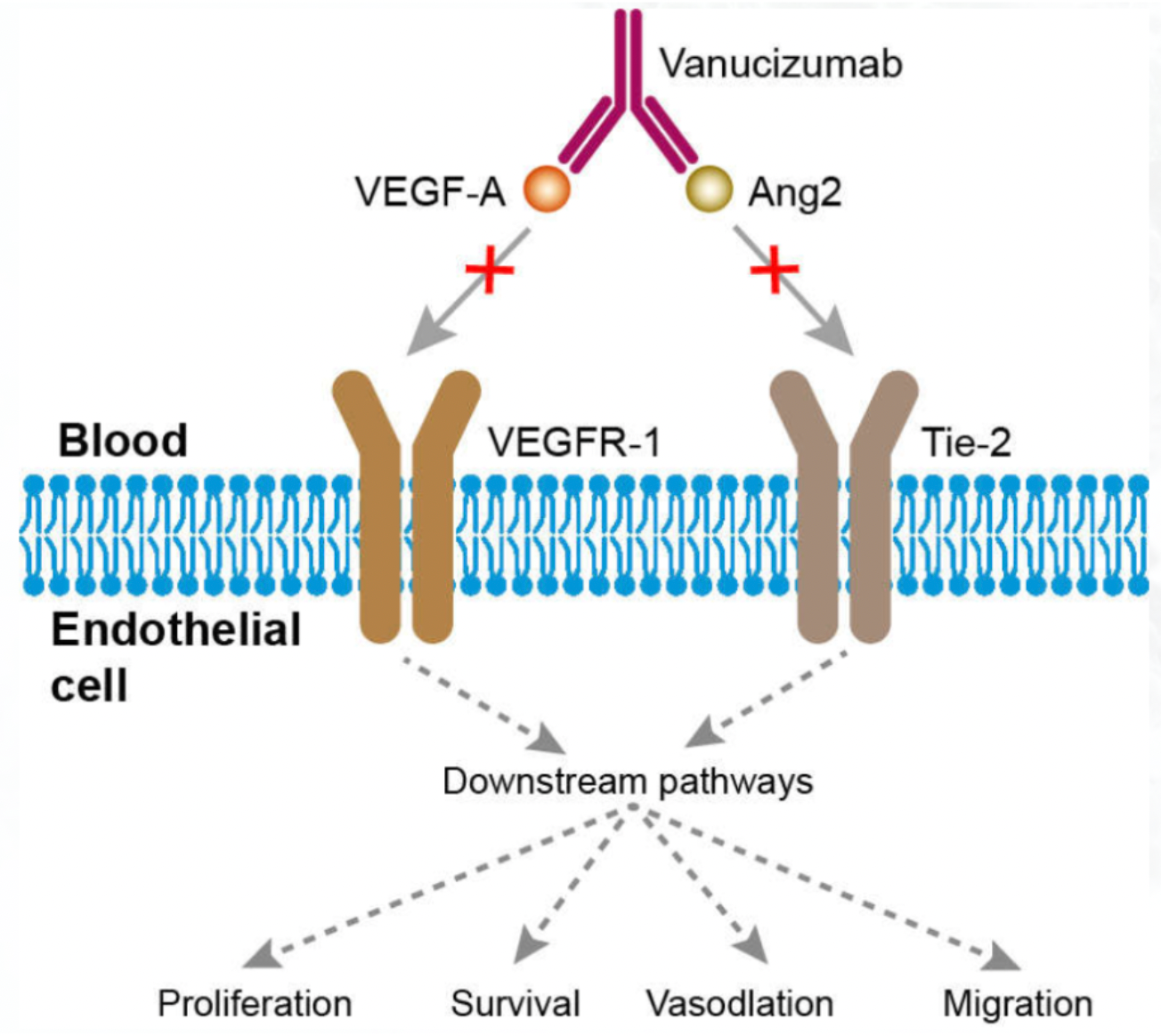
Ligand-Receptor Inhibitory bsAbs: Ligand-receptor inhibitory bispecific antibodies (bsAbs) block signal transduction by interfering with the binding of ligands to their receptors or by inhibiting receptor homodimerization. For example, bispecific antibodies targeting VEGF and ANG2 can simultaneously blockade the VEGFR and TIE2 pathways, both of which promote angiogenesis, thereby suppressing tumor growth and metastasis.
Vanucizumab is one such bsAb that concurrently inhibits the biological activities of two different biomolecules, VEGF-A and angiopoietin-2 (ANG2). VEGF and ANG2 are cytokines that play key roles in the genesis and progression of tumors by activating their respective receptor pathways to stimulate tumor neovascularization, which in turn supports tumor growth, invasion, and metastasis. In preclinical model studies, vanucizumab has demonstrated significant anti-tumor, anti-angiogenic, and anti-metastatic activities.
Similarly, BI836880 is a trispecific nanobody-based fusion protein comprising three distinct nanobodies that respectively target VEGF (Vascular Endothelial Growth Factor), ANG2 (Angiopoietin-2), and HSA (Human Serum Albumin). The design of this drug aims to inhibit tumor growth and spread by simultaneously blocking VEGF and ANG2, two key signaling pathways involved in tumor angiogenesis. The portion that binds to HSA is intended to extend the drug's half-life in the human body, ensuring a more prolonged therapeutic effect.

Receptor-Activated bsAbs: Activating bi-specific antibodies (bsAbs) function by promoting the formation of effective clusters of specific receptors to activate their downstream signaling pathways, such as targeting the members of the TNFRSF family and their receptors.
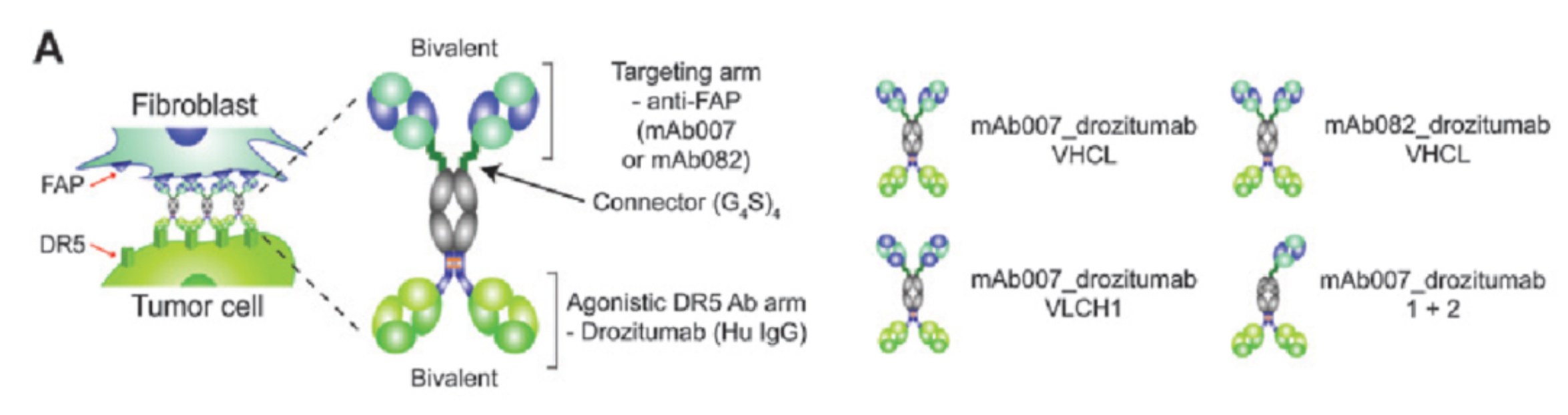
For example, RO6874813 (also known as RG7386) is a tetravalent bi-specific antibody designed to target cancer-associated fibroblasts (CAFs) surface Fibroblast Activation Protein-alpha (FAPα) and Death Receptor 5 (DR5). FAPα is highly expressed in the Tumor MicroEnvironment (TME), particularly on CAFs associated with tumor progression and metastasis. DR5, a member of the TNF superfamily, can initiate apoptosis in cancer cells when activated by a specific ligand like TRAIL. RO6874813, by binding to both FAPα and DR5, can efficiently direct pro-apoptotic signals to tumor cells and enhances the selectivity and potency toward DR5 by avoiding degradation or inactivation caused by endogenous or exogenous decoy receptors. In experimental studies, this drug has demonstrated strong selectivity and in vivo antitumor activity, effectively killing tumor cells in FAPα-positive mouse models, and therefore it has great potential as a novel anti-cancer therapy.
BsAbs for Directed Payload Delivery: BsAbs designed for targeted payload delivery typically employ two strategies: one is pretargeted therapy, which initially uses one binding site to deliver the drug to the tumor site, followed by the capture of a radiolabeled payload or drug complex with another site; the other involves directly linking toxins or radioactive isotopes to the bsAb to selectively kill cancer cells. For example, a bsAb targeting CEACAM5 or HER2 can carry a radioactive isotope, delivering it precisely to the tumor tissue.
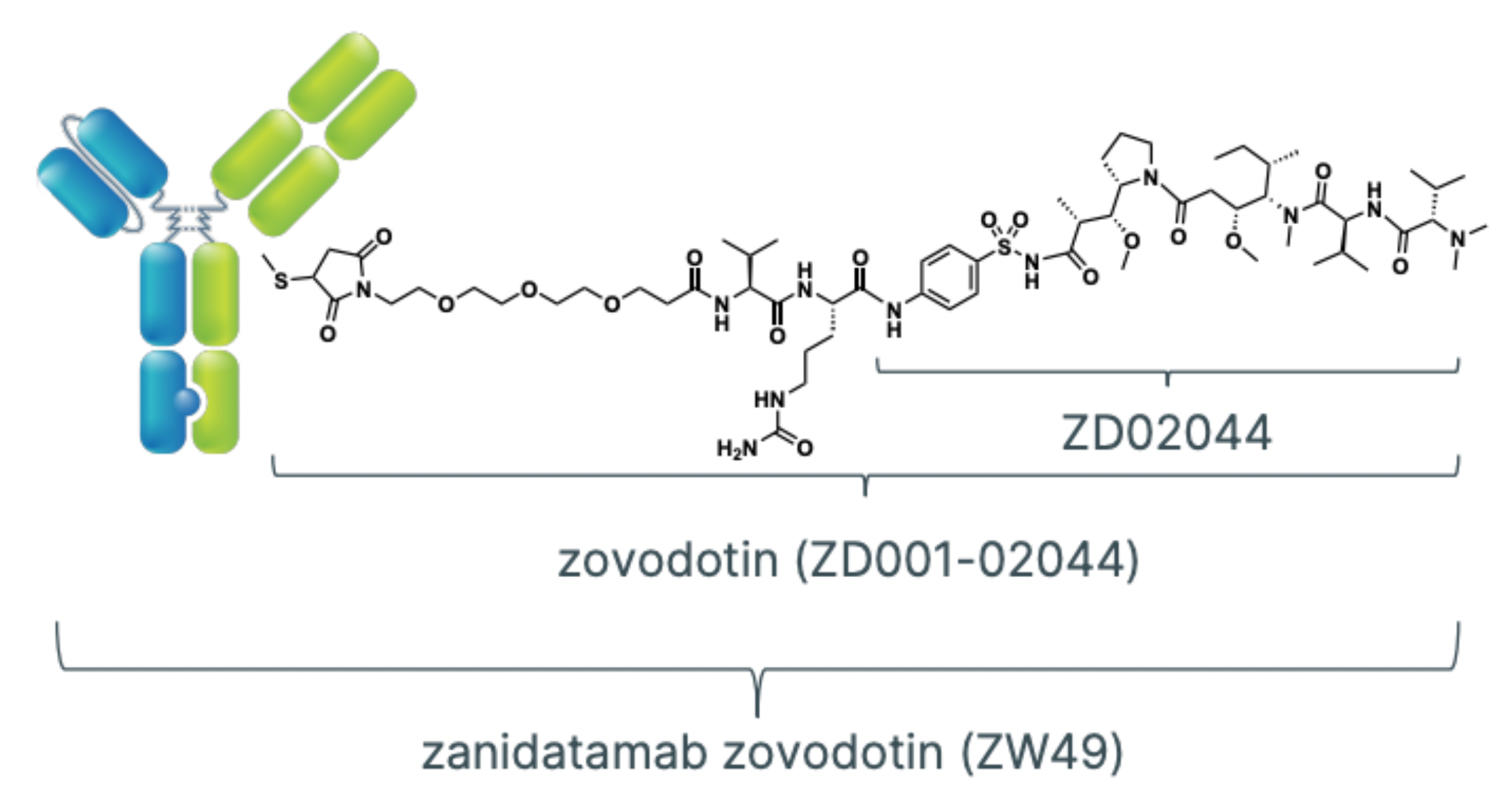
For instance, zanidatamab zovodotin (ZW49) is a bispecific antibody-drug conjugate (bsADC) that combines a bispecific antibody targeting the HER2 receptor with a cytotoxic payload derived from Auristatin. Zanidatamab is the core component of this ADC, capable of binding different epitopes on the HER2 receptor concurrently. This biparatopic (dual-epitope targeting) mechanism helps to enhance the affinity for HER2-positive tumor cells and to form more stable and functionally potent HER2 complexes. ZW49 leverages this bispecific structure to precisely target cancers that express or amplify HER2, especially because once the auristatin-derived cytotoxin is conjugated, it can release its cytotoxic payload inside tumor cells upon entry, thereby exerting a cytotoxic effect and killing cancer cells.
Other Bispecific Antibodies (bsAbs) for Cancer Treatment: The mechanisms of action of most bispecific antibodies (bsAbs) used in cancer immunotherapy can be broadly classified into two categories. One category works by enhancing the natural or endogenous immune response driven by T cells, for example, by amplifying existing anti-tumor responses or overcoming immune checkpoint inhibition. The other category functions by providing synthetic immunity, such as through bsAb-mediated recruitment, activation, and interaction of immune cells. The article also overviews the most prominent mechanisms of action of bsAbs and multispecific antibodies, covering a variety of molecular design strategies including immune checkpoint inhibitors (CPIs), effector cell engagers, and co-stimulatory bsAbs.
Dual Checkpoint Inhibitors (Dual CPIs): In cancer immunotherapy, bispecific antibodies are used to block two different immune checkpoint proteins simultaneously, to more effectively relieve the suppression of T cell activity by tumors. For instance, designed bsAbs can target checkpoints like PD-L1 and CTLA4 at the same time.
Effector Cell Engagers: These bsAbs are designed to directly connect tumor cells to immune effector cells, such as natural killer cells (NK cells), macrophages, and dendritic cells (DCs), to promote the recognition and elimination of tumor cells by effector cells. For example, some bsAbs can bind to receptors such as NKp46 or NKp30 alongside tumor-associated antigens, thereby enhancing the NK cells' cytotoxic action against tumors; others operate by targeting CD3 molecules to engage T cells with tumor cells expressing specific antigens, like BiTEs and T-cell engagers.
Co-stimulatory bsAbs: These bispecific antibodies are designed to simultaneously activate two co-stimulatory receptors in the immune system to enhance the immune response. For instance, FS120 is a tetravalent bsAb targeting 4-1BB and OX40, which can effectively activate T cells and generate anti-tumor activity, while avoiding the hepatic toxicity issues possibly caused by agonistic 4-1BB monoclonal antibodies alone. Additionally, there is a bivalent bsAb targeting 4-1BB and CD40 (tecaginlimab), which not only activates T cells but also induces a robust CD8+ T cell-mediated immune response by activating dendritic cells (DCs).
MDCs and Dendritic Cell-Activating bsAbs: Some bsAbs are designed to specifically bind to markers on the surface of myeloid dendritic cells (MDCs) or DCs, such as Clec12a, for the precise delivery of immune activation signals. They activate DCs and improve their antigen-presenting capabilities, thereby triggering a potent CD8+ T cell immune response.
Tumor-Targeting Co-stimulatory bsAbs: These antibodies are engineered to target specific antigens on tumor cells while activating co-stimulatory receptors of the immune system. For instance, bsAbs against CD47 can block the "don't eat me" signal, making tumor cells more susceptible to recognition and clearance by phagocytic cells. In addition, they can recruit other effector cells through the Fc region, increasing the aggressiveness towards the tumor.
Innate Immune Cell Engagers and T Cell Engagers: These bispecific antibodies (bsAbs) are designed to activate and direct natural killer (NK) cells and T cells to tumor cells. Some of these bsAbs retain or enhance the binding ability to FcγRIII to ensure the effective participation of NK cells; while others incorporate cytokines such as IL-2 or IL-15 into the bsAb structure to expand and activate the innate immune cell population.
PROTAC bispecific antibodies (bsAbs): This is a molecular drug that combines the technology of proteasome-mediated protein degradation with traditional bispecific antibody design strategies. These antibodies promote the tagging of target tumor-associated proteins with ubiquitin by simultaneously binding to E3 ubiquitin ligases or other factors capable of triggering internalization and subsequent degradation processes (such as membrane-accessible E3 ubiquitin ligases or transferrin receptors), leading to their degradation in the proteasome. Compared to traditional antibody therapies that only block signaling pathways to inhibit tumor cell growth, PROTAC bsAbs achieve a more thorough intervention by degrading target proteins, effectively addressing treatment failure due to drug resistance. Although this field is still in the early stages of development and no PROTAC bsAb has entered the clinical research phase, their design concept is compatible with the development of "standard" bispecific antibodies and provides a unique possibility for exploring new anti-cancer approaches. In the future, with further research and technological development, PROTAC bsAbs are expected to become a potent, highly selective, and targeted cancer treatment method.
Moreover, the article provides a detailed description of the design features of different bispecific antibody (bsAb) structures, such as using an IgG-like structure and ensuring the correct assembly of heavy chains and light chains through techniques like the "knobs-into-holes" technology and Fab-arm exchange (cFAE). It also discusses engineering modifications to the Fc region to attenuate or eliminate the binding to Fcγ receptors and complement, hence reducing nonspecific effects. The article also introduces the use of bsAbs to stimulate members of the TNFRSF family (e.g., DR4 and DR5) as potent and tumor-selective agonists. By designing bispecific antibodies that target tumor-associated antigens and TNFRSF members, efficient anti-tumor effects are achieved. It is noted that this mechanism is also applicable to costimulatory molecules that depend on receptor clustering for activation, such as 4-1BB, OX40, and CD40.