What Does Tirofiban Do?
Tirofiban, marketed under the brand name Aggrastat, is a potent medication that belongs to the class of glycoprotein IIb/IIIa receptor inhibitors. It is primarily used to prevent blood clots and heart attacks in patients experiencing severe chest pain or undergoing a procedure known as angioplasty, which is used to open blocked arteries. Developed by Merck & Co., tirofiban has been a significant advancement in the management of acute coronary syndrome. The drug is administered intravenously and is not suitable for oral use due to its rapid metabolism in the gastrointestinal tract.
Mechanism of Action of Tirofiban
Tirofiban exerts its effects by binding to the glycoprotein IIb/IIIa receptors on the surface of platelets, which are essential for platelet aggregation—the process that leads to blood clot formation. By inhibiting these receptors, tirofiban reduces the ability of platelets to stick together and form a clot, thus decreasing the risk of thrombotic events in patients with acute coronary syndrome.
How to Use Tirofiban
Tirofiban is administered as an intravenous solution through a vein by a healthcare provider. The typical dosing regimen for acute coronary syndrome includes an initial dose of 25 mcg/kg infused over 5 minutes, followed by a maintenance dose of 0.15 mcg/kg/min for up to 18 hours. It is crucial for patients to receive this medication under medical supervision due to the risk of bleeding and other serious side effects. While using tirofiban, patients may require frequent blood tests to monitor its effects and check for any adverse reactions.
Side Effects of Tirofiban
Tirofiban can cause a range of side effects, with the most significant being an increased risk of bleeding. This can present as easy bruising, nosebleeds, bleeding gums, or bleeding around the IV or catheter site. Internal bleeding, such as in the stomach or intestines, can also occur and may manifest as bloody or tarry stools, coughing up blood, or vomiting material that looks like coffee grounds. Other common side effects may include dizziness, slow heart rate, leg pain, pelvic pain, and increased sweating or swelling.
Contraindications and Precautions
Tirofiban is contraindicated in patients with active internal bleeding, a history of bleeding or blood-clotting disorders, a history of low blood platelets after treatment with tirofiban, or those who have had recent surgery, injury, or medical emergency within the past 30 days. Patients should inform their doctor if they have kidney disease, are pregnant or planning to become pregnant, or are breastfeeding.
Drug Interactions with Tirofiban
Tirofiban may interact with various other medications, increasing the risk of bleeding or altering its effectiveness. Patients should inform their doctor about all medications they are taking, especially antiplatelet drugs like clopidogrel and ticlopidine, anticoagulants like dalteparin, enoxaparin, tinzaparin, desirudin, dabigatran, fondaparinux, dipyridamole, or warfarin. The use of nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin, ibuprofen, naproxen, celecoxib, diclofenac, indomethacin, or meloxicam should be discussed with a doctor, as they may increase the risk of bleeding when taken with tirofiban.
In conclusion, tirofiban is a valuable treatment option for patients at risk of blood clots and heart attacks. However, due to its potential to cause severe bleeding and other side effects, it must be used with caution and under the strict supervision of healthcare professionals. Patients receiving tirofiban should be closely monitored and follow all medical advice to ensure safe and effective treatment.
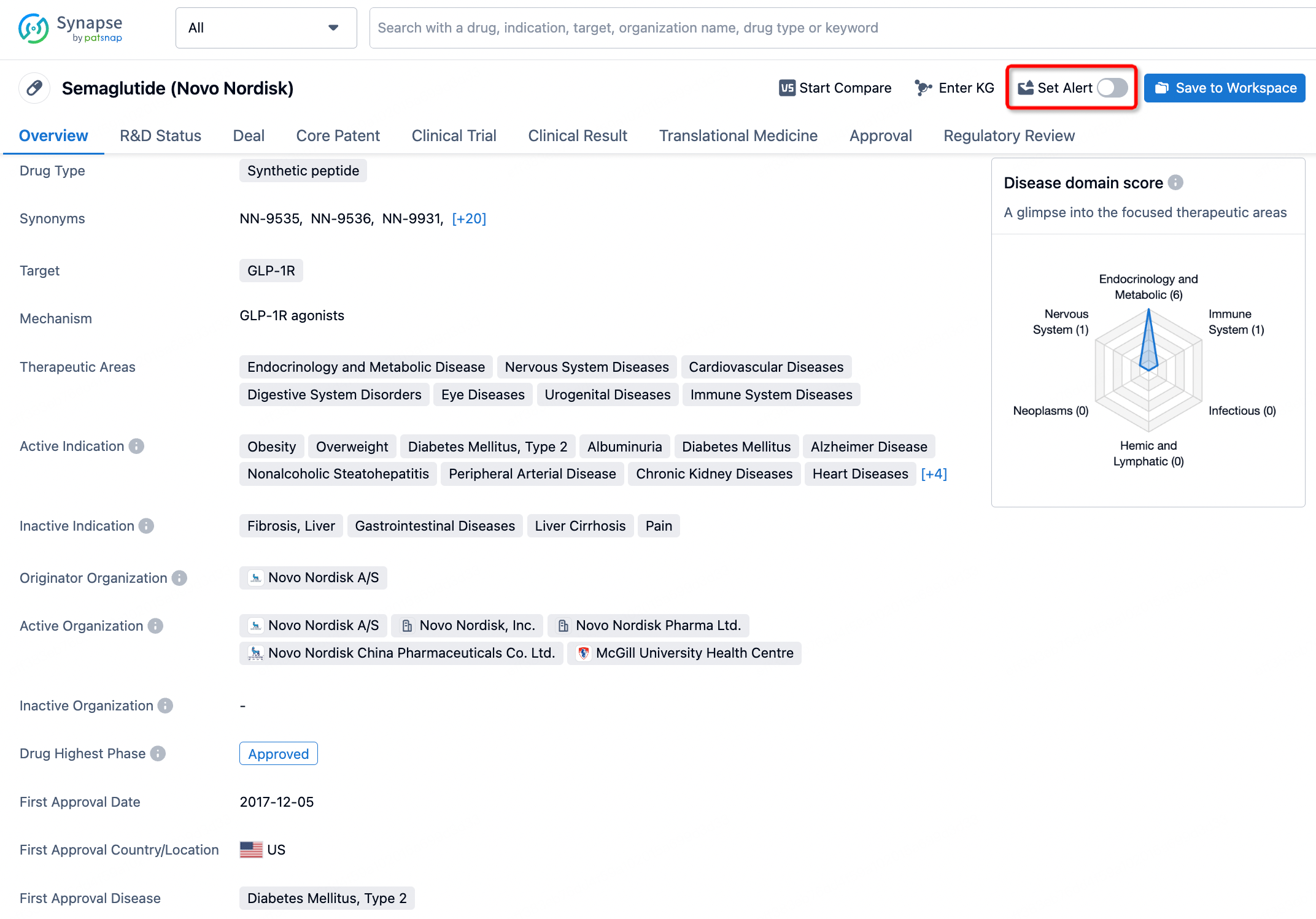
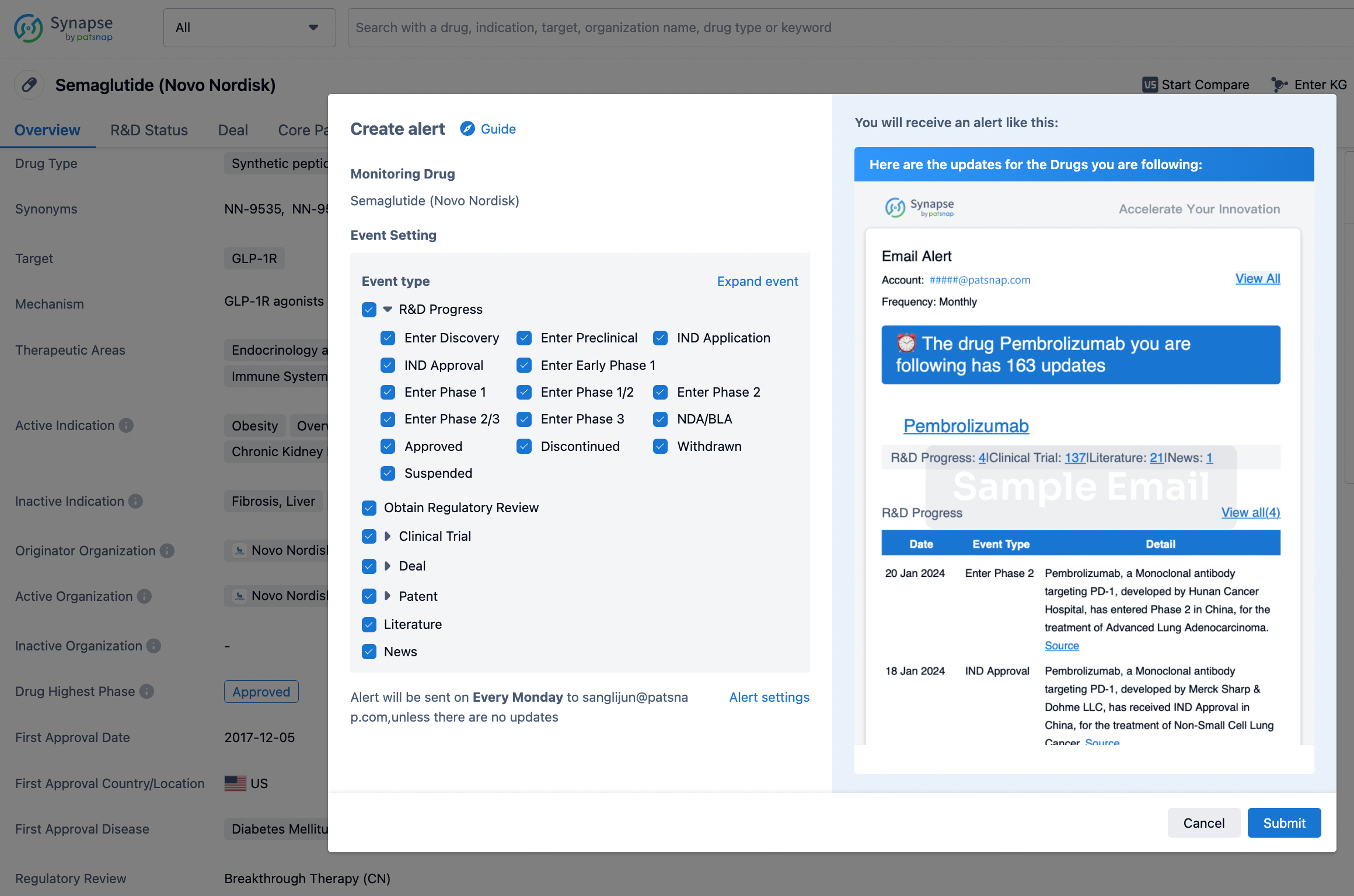
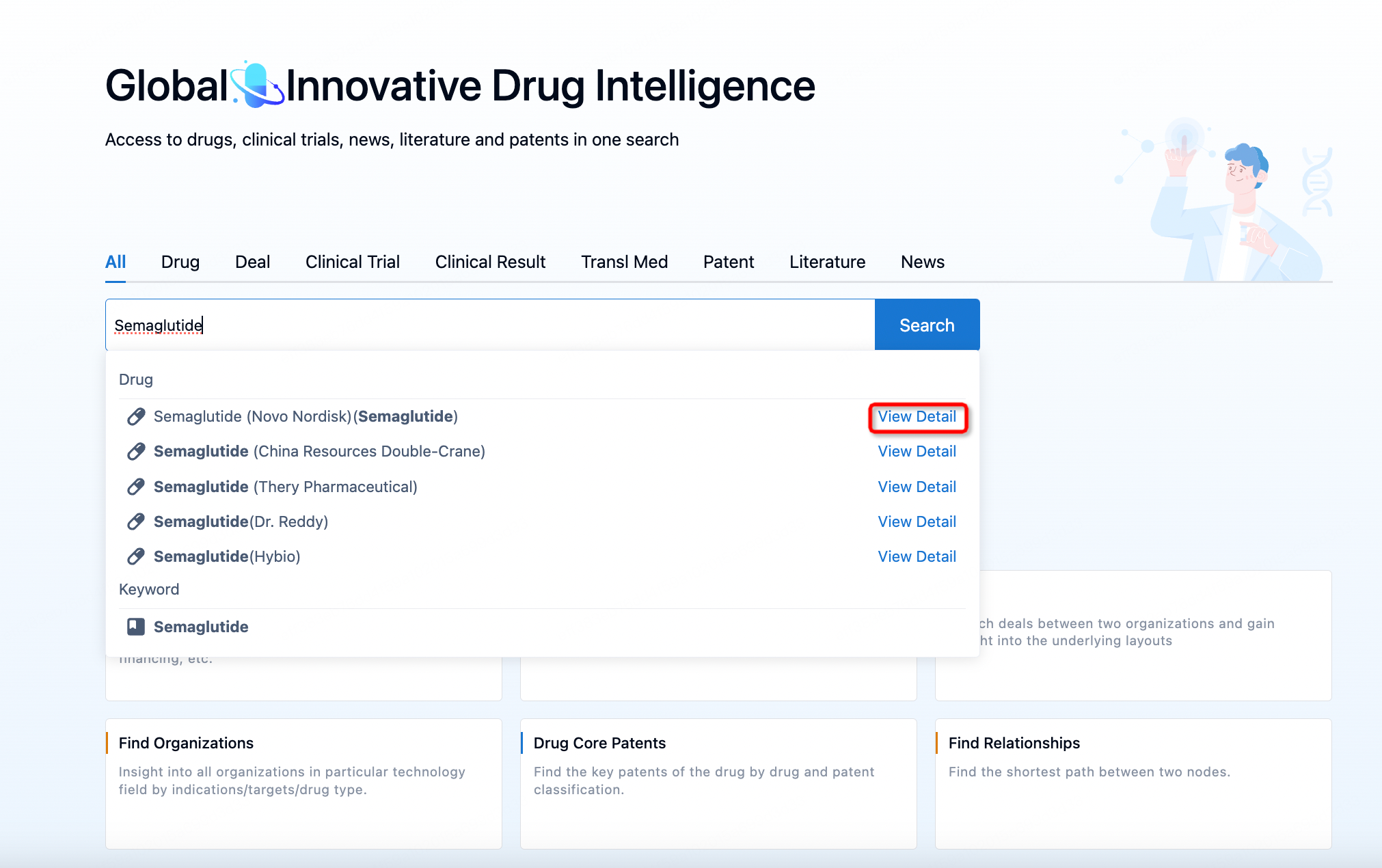
How to obtain the latest development progress of all drugs?
In the Synapse database, you can keep abreast of the latest research and development advances of all drugs anywhere and anytime, daily or weekly, through the "Set Alert" function. Click on the image below to embark on a brand new journey of drug discovery!